Overview
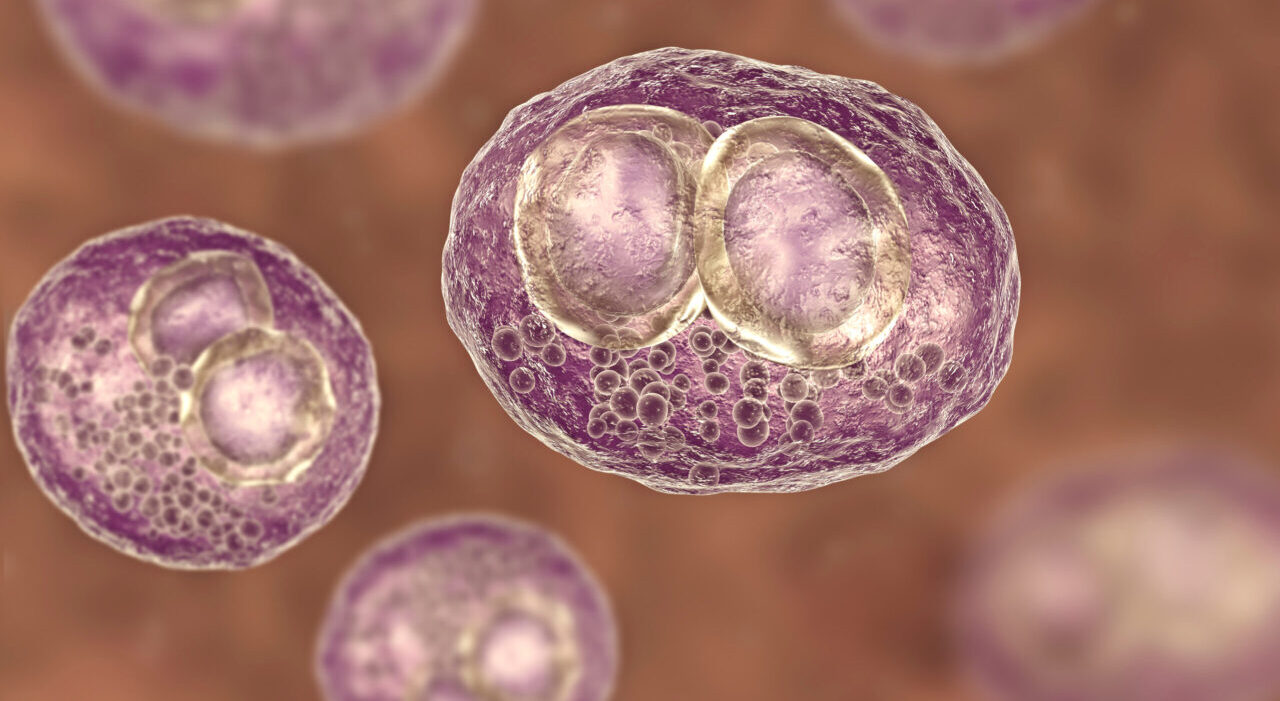
My laboratory studies the strategies that viruses use to escape detection by our immune system. These strategies facilitate viral replication, and in some cases help them establish lifelong infections that we can never clear. We are intrigued by virus-employed tricks that target members of the tumor necrosis factor (TNF) family, as these proteins released by our immune cells are fundamentally important in fighting infection. We also have a particular interest in cytomegalovirus (CMV), which is a member of the herpesvirus family similar to ‘mono’ (Epstein-Barr) and the chicken pox/shingles (Varicella Zoster) viruses. CMV encodes one of the largest known viral genomes (~230,000 base pairs), and more than half of it is dedicated to throwing up smoke screens that fool our immune systems, including many that block the TNFs. We believe that studying the unique CMV strategies that allow it to evade detection by our immune system facilitates fundamental new discoveries about our health. In addition, our lab is focused on finding new ways to combat the diseases that CMV can cause in certain settings. CMV is the No. 1 infectious cause of birth defects in the U.S. today, causing severe disease if immunity is naïve or compromised (e.g. infection of babies in the womb and transplant patients), and we are developing new vaccine strategies to combat this. If you have a healthy immune system, CMV infection is largely benign. However, like the chicken pox that can reemerge 50 years later to cause shingles, CMV ‘hides’ in your body for life and can pop-out again when your immune system is weakened or older. Consequently, CMV is a likely contributor to auto-inflammatory disorders such as vascular disease and immune senescence, and may even contribute to some cancers. One of our recent discoveries could aid efforts in the development of a CMV vaccine.
Featured publications
Cytomegalovirus evades TRAIL-mediated innate lymphoid cell 1 defenses
Cytomegalovirus: shape-shifting the immune system
A noncanonical function of cGAMP in inflammasome priming and activation
Lab Members
 CB
CB
Christopher Benedict, Ph.D.
Associate Professor Center for Autoimmunity and Inflammation, Center for Vaccine InnovationResearch Projects
CMV Interfaces with The Trail Cytokine System
We have recently discovered a novel connection between the TNF-related apoptosis inducing ligand (TRAIL) cytokine system and CMV. TRAIL is
CMV Targets the Immune Checkpoint Inhibitor BTLA
Virulent isolates of CMV encode the ul144 orf, and we identified UL144 as an orthologue of the herpesvirus entry mediator
T Cell Immunity and CMV
HCMV-specific CD8 T cells protect bone marrow transplant patients when used in cellular immunotherapy, and their long-term maintenance is enhanced
The Lymphotoxin-Interferon Antiviral Immunity Axis
Over the last 15 years our lab has been studying the link between lymphotoxins (LT) and the regulation of type
From the lab

Know Your Enemies
They help us digest food, balance our immune system, and keep our hearts and brains healthy. But harmful viruses and
Q&A with Dr. Benedict
As a scientist Chris Benedict, Ph.D., came of age during the heyday of gene therapy. But when the first clinical
Researchers advance fight against leading infectious cause of congenital birth defects
SAN DIEGO – March 13, 2013 A virus most people probably have never heard of, but that the majority of
Awards & Honors
- Arthritis National Research Foundation Eng Tan Scholar, 2006
- American Heart Association ‘Promising Young Scientist’ (recipient of Scientist Development Grant), 2001
- Smoot Pre-Doctoral Fellow, 1992