Overview
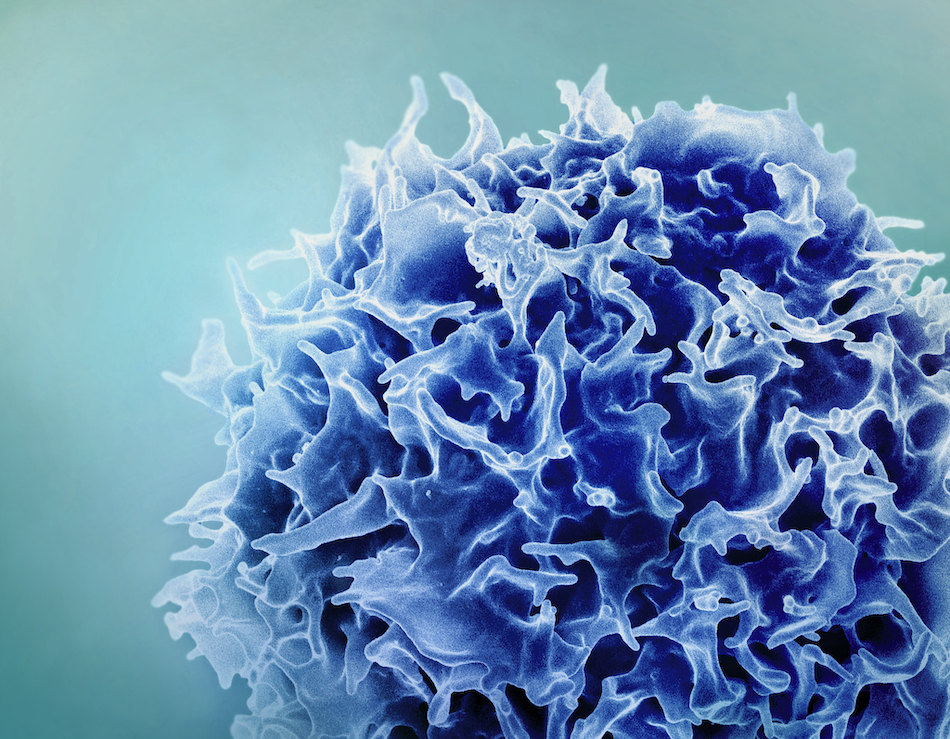
Hilde Cheroutre, Ph.D., and her team are studying the development, function, and regulation of white blood cells, a type of T lymphocytes. The laboratory is investigating how the immune system provides protection at “interfaces,” or places where the outside world comes in contact with the inside of the body, such as skin, lungs, mouth, and the largest surface of all, the intestine.
Studying how the immune system works in the intestine is of particular interest because the immune system has to be able to distinguish pathogenic antigens from harmless food peptides and bacteria. The laboratory is investigating how the immune system succeeds in differentiating between the two and what causes the system to fail, allowing the antigens to invade the body.
The lab’s research has been expanded to studying immune memory cells that resist re-entering pathogens or cancer cells. Tumor cells produce tumor antigens, which are cell surface proteins that differ from the proteins expressed by the surrounding normal cells. White blood cells recognize and destroy these transformed cells. Some of these tumor-fighting white blood cells go on to become immune memory cells. These are long-lived cells that activate immediately when they re-encounter tumor antigens, in the case of metastasis or re-occurrence of the tumor.
Understanding the function of immune memory T cells will help in the development and improvement of effective vaccines. At the same time, the ability to specifically eliminate these cells is a key requirement in the therapeutic intervention against autoimmune diseases and the rejection and/or destruction of host tissue following transplantation.
Lab Members
 HC
HC
Hilde Cheroutre, Ph.D.
Professor Center for Autoimmunity and Inflammation, Center for Cancer ImmunotherapyResearch Projects
CD4+ Cytotoxic Lymphocytes
MHC class-II restricted CD4+ T cytotoxic cells (CD4 CTL) are among the best examples of extreme measures the immune system
Mechanisms Involved in The Generation of High Affinity Effector Memory T Cells
A hallmark of immune memory is that repeated infections are met with accelerated or/and enhanced protective immunity. Furthermore, unlike naive
Mucosal CD4- CD8- T Cells
One large subgroup of specialized T cells is encompassed by the intraepithelial T cells which are located in the epithelium
Regulation of mucosal immunity by stromal cells and dendritic cells crosstalk in the gut
Genetic regulation by vitamin A is involved in multiple biological processes such as embryonic development, vision, and immunity. To exert
Role of Pre-TCR Signaling in Central Tolerance and Autoimmunity?
Autoimmunity is a self-destructive disease condition mediated mainly by pathogenic selfreactive αβ T cell receptor (TCR) expressing T lymphocytes. Self-tolerance
T Cell Function
We are now trying to elucidate the regulatory functions displayed by the self-specific agonist selected T cells and their role
From the lab
New LJI research has major implications for controlling T cell activity
How a supposed "nuclear" receptor makes TCR signaling possible

Origin story: How T cell heroes and villains are made
LJI Postdoctoral Fellow Greet Verstichel on how T cells learn their "fate"
Amazing mucosa
“The whole mucosal immune system is so fascinating. It has to operate in an environment of extremes.”
Awards & Honors
- NIH Director’s Pioneer Award Recipient 2009
- UCSD Warren Foundation Celiac Disease Grant
- Cancer Research Coordinating Committee Fellowship from the State of California
- University of California, Los Angeles Tumor Cell Biology Training Grant
- Markey Foundation Postdoctoral Fellowship
- NATO Postdoctoral Fellowship (Awarded Twice)