Coronavirus is a respiratory virus that commonly causes cold- and flu-like symptoms. It is present throughout the world, though outbreaks of new strains have occurred in the recent past. Since late 2019, a new strain has been identified as part of an outbreak in Hubei Province, China (“2019-novel coronavirus” or “SARS-CoV-2”).
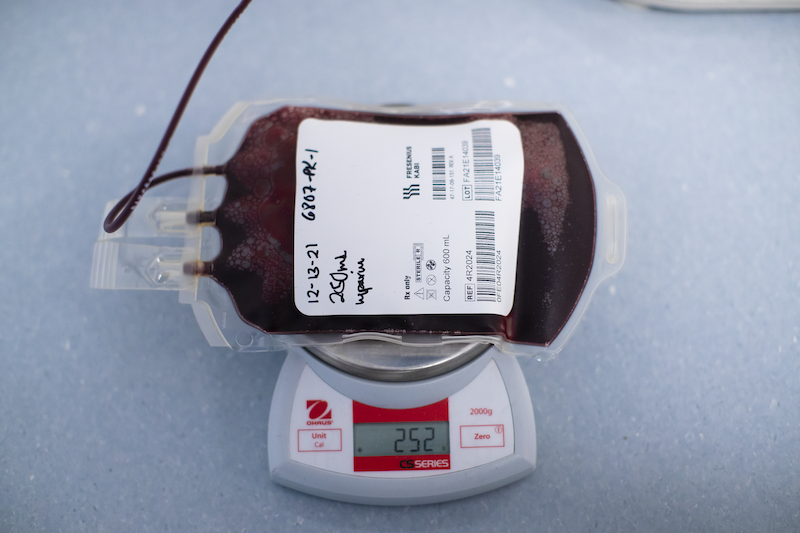
As more and more people become infected with this new strain of the virus, it is important to understand as much as we can about how this strain of the virus affects the human immune system. We plan to look at the T and B cell immune response in patients with symptoms and history of COVID-19 disease as well as in healthy controls.
Eligibility Criteria (one or more):
- You are a generally healthy male or female, over 18 years of age.
- You have had a positive test for COVID-19.
- You have been vaccinated for COVID-19
- You have had a “breakthrough” infection of COVID-19 after being vaccinated