Scientists in the La Jolla Institute for Immunology (LJI) Coronavirus Task Force remain at the forefront of research into COVID-19 vaccines, therapies and the disease’s long-term effects.
T Cell Breakthroughs
In January 2020, LJI scientists began studying T cell reactivity to the SARS-CoV-2 virus. Their findings gave the world early evidence that the immune system could indeed fight off the virus, offering hope that a vaccine could be effective.
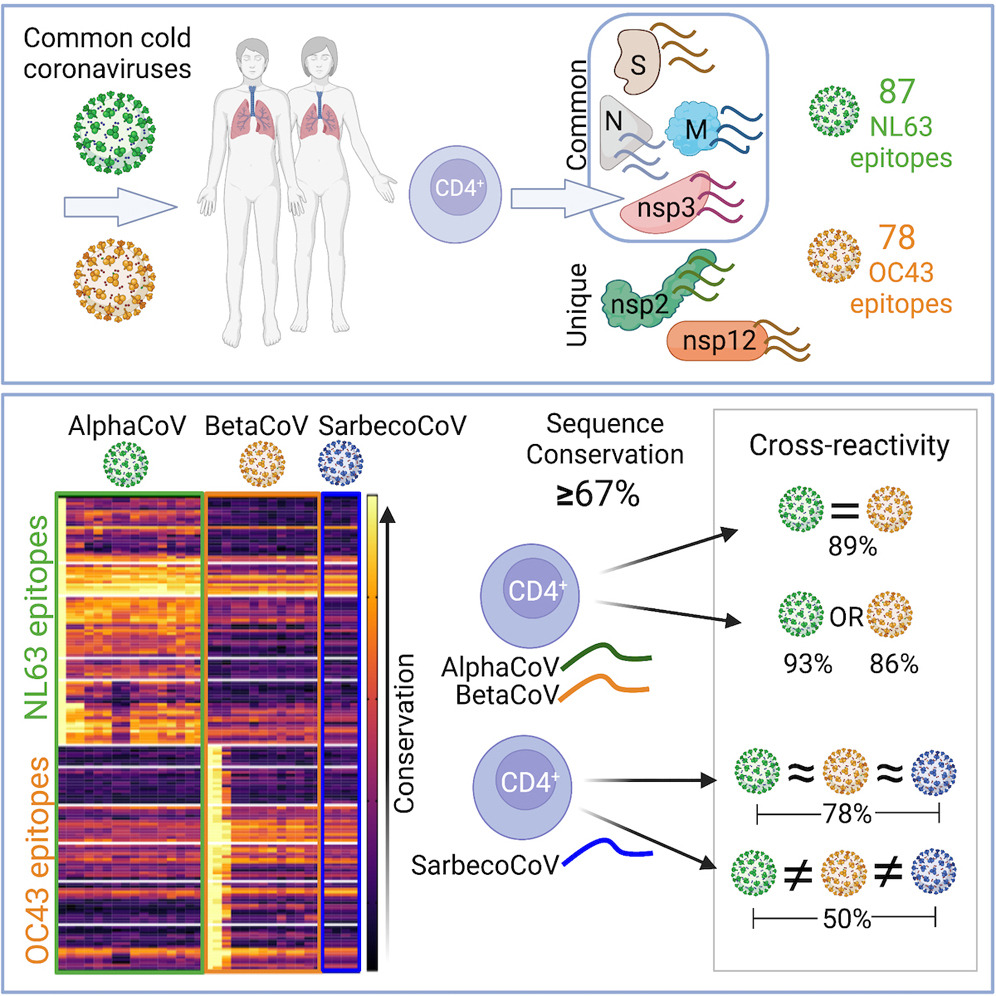
LJI Professors Alessandro Sette, Dr.Biol.Sci., and Shane Crotty, Ph.D., continued this groundbreaking research throughout 2020 and 2021. Their labs were the first to share a detailed analysis of the body’s adaptive immune response to the virus. Importantly, they showed that people who had previously had common cold coronaviruses had “cross-reactive” T cells that also recognized SARS-CoV-2. Their labs also found that a dysfunctional T cell response could explain the huge variation in COVID-19 outcomes, especially in the elderly.
LJI Professor Pandurangan Vijayanand, M.D., Ph.D., worked with scientists at the University of Liverpool and the University of Southampton to show that people with severe COVID-19 cases may be left with more of the protective “memory” T cells needed to fight reinfection. The Vijayanand Lab also found that early in the illness, patients hospitalized with severe cases of COVID-19 develop a novel T cell subset that can potentially kill B cells and reduce antibody production.
Vaccine Findings
By early 2021, the Task Force had shown that COVID-19 survivors held on to SARS-CoV-2 immunity for at least eight months. The Crotty and Sette Labs then found that Pfizer-BioNTech and Moderna vaccines effectively prime T cells to fight SARS-CoV-2 variants. A key study co-led by LJI Instructor Alba Grifoni, Ph.D., showed exactly how these T cells can mount attacks against many SARS-CoV-2 targets—even on new virus variants. This work was key for understanding how people around the world may respond to emerging SARS-CoV-2 variants.
LJI Research Assistant Professor Daniela Weiskopf, Ph.D., co-led research suggesting even a low dose of the Moderna vaccine lasts for at least six months. This study, published in September 2021 in Science, also showed that cross-reactive T cells from previous common cold coronavirus infections can help a vaccinated person fight the virus.
Antibody Therapeutics
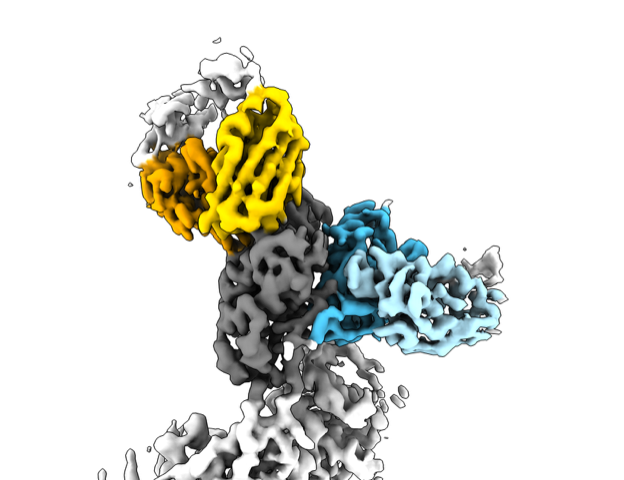
LJI President and CEO Erica Ollmann Saphire, Ph.D., launched the Coronavirus Immunotherapeutic Consortium (CoVIC), with backing from the Bill & Melinda Gates Foundation in 2020. With more than 50 different efforts currently underway to find therapeutic antibodies across the globe, CoVIC provides a coordinated and standardized effort to compare these antibody candidates side by side. In September 2021, CoVIC published a study in Science highlighting key details of where SARS-CoV-2 is vulnerable and which antibody “all stars” could be combined in life-saving therapies.
Global Studies
In early summer 2020, work between the Saphire Lab and researchers at Los Alamos National Laboratory also gave us an early look at how SARS-CoV-2 was mutating as it spread across the globe, alerting many to the development of viral variants.
LJI Professor Sujan Shresta, Ph.D., won funding in February 2021 to study the spread of COVID-19 in Nepal, Vietnam and the Philippines. These new projects will shed light on how infectious diseases spread in these countries—and how differences in geography and genetics affect immune responses.
In addition to applying his bioinformatics expertise for T cells studies, LJI Professor Bjoern Peters, Ph.D., also weighed in on the hypothesis that BCG vaccination provides immunity from SARS-CoV-2, which was based on—in his opinion—incorrectly interpreted early epidemiological data of how the pandemic spread. His work emphasized the importance of open and critical scientific debate, especially in light of a pandemic.
Vascular symptoms and long COVID
LJI Professor Catherine “Lynn” Hedrick received $523,914 in funding from the National Institutes of Health’s National Heart, Lung, and Blood Institute (NHLBI) in October 2020 to study how immune cells called monocytes may contribute to cardiovascular problems in COVID-19 patients. The Hedrick Lab has also built a new team of clinical and basic science experts from around the world to study the long-term heart and lung complications arising from SARS-CoV-2 infection.
Dr. Sonia Sharma established new collaborations to study children afflicted with MIS-C, also called Pediatric Multisystem Inflammatory Syndrome. She and her team are using samples collected from children and adults in the Los Angeles area to examine whether the same immune-related metabolic mechanisms underlie multi-organ inflammation and vasculitis in children with MIS-C.
Dr. Peters and team have been working on data standardization and analysis for the largest NIH study of COVID-induced immune responses to date. His lab has been following patients for over 12 months to track the effects of COVID infections, including long COVID.
A new lab and clinical center
In the summer of 2020, LJI opened the donor-funded Infectious Disease Exploration and Abatement (IDEA) Facility, a biosafety level 3 lab. Scientists at LJI require this level of containment to safely study the virus that causes COVID-19, as well as other highly infectious threats. This research could lead to better diagnostics and vaccine strategies for many diseases.
LJI also celebrated the opening of the John and Susan Major Center for Clinical Investigation in May 2021. Thanks to a generous gift from local philanthropists, John and Susan Major, the new space greatly expands the Institute’s capacity to collect human blood samples for studies into COVID-19 and other diseases.
Going Forward
The LJI Coronavirus Task Force is building on these accomplishments and looking forward as work remains to better understand SARS-CoV-2 and treat COVID-19, to identify and fight new mutations, and also be prepared for future pandemics.
In May 2021, Dr. Shresta established a partnership with Synbal, Inc., a preclinical biotechnology company based in San Diego, California, to develop multi-gene, humanized mouse models for COVID-19 research. These more complex mouse models are expected to give scientists a window into why SARS-CoV-2 causes a range of disease severities and why some people develop “long COVID.” They may also be good models for testing antibody-based therapeutics against COVID-19 and “next-generation” vaccines that protect against SARS-CoV-2 variants and future emerging coronaviruses.
Dr. Weiskopf has been granted $1.4 million from the National Institutes of Health’s National Cancer Institute (NCI) to examine the immune response to SARS-CoV-2 in study volunteers from Puerto Rico, where at least 75 percent of the population identifies as Hispanic or Latino.
LJI Postdoctoral Associate Sydney Ramirez, Ph.D., won a three-year fellowship from the A.P. Giannini Foundation to study adaptive immunity to SARS-CoV-2. She wants to know how the development of SARS-CoV-2-specific B cell and T cell immunity in acute cases of COVID-19 correlates with viral loads, symptoms and disease severity.