LA JOLLA, CA—When a massive Zika virus outbreak swept through South and Central America and the Caribbean in 2016, thousands of children exposed to the virus during pregnancy were born with severe neurodevelopmental problems. Although new infections have since drastically declined, researchers around the globe are racing to understand the interactions between the virus and its host, and most importantly, to develop a preventative vaccine.
The latest study by researchers at the La Jolla Institute for Immunology (LJI) and their collaborators provide the first in-depth characterization of the body’s cytotoxic T cell response to Zika, which plays an important role in providing protective immunity against Zika. By revealing that Zika induces a fully functional cytotoxic T cell response, their findings provide a valuable snapshot of what a protective immune response to a potential vaccine should look like.
“Whether Zika will make a comeback is not a question of if but when, and there is great concern about neurological complications caused by Zika infections such as severe birth defects and in adults, Guillain-Barré syndrome,” said LJI professor Alessandro Sette, Dr. Sci. Biol., who led the study published in early online edition of The Journal of Immunology. “Cytotoxic T cells are an important component of protective immunity against Zika and it is essential to know whether these responses are somehow altered since they could contribute to immunopathology.”
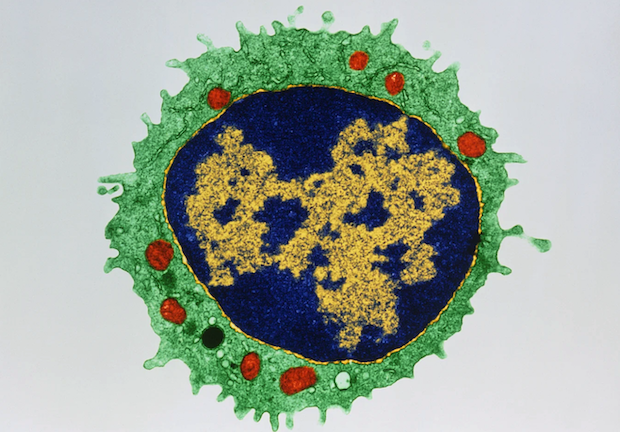
When a virus invades a host, some T cells help stimulate antibody production. Others, known as cytotoxic T cells or CD8 T cells for the CD8 molecule on their surface, kill virus-infected cells either directly or through the production of cytokines that signal other cells. Once the virus has been fended off, a small number of so-called memory B and T cells persist and can be reactivated at a moment’s notice and fend off a new infection before it can gain a foothold. Vaccines harness the immune system’s ability to retain a “memory” to stimulate long-term protection by presenting inactivated viruses or virus components to the immune system without causing an active infection.
Recent advances in technology and data analysis allow scientists to study the activity of these immune cells across diverse populations around the globe to trace the markings of a successful immune response in great depths. With funding from the Human Immunology Project Consortium (HIPC) and additional support from the Zika Preparedness Latin American Network (ZikaPLAN), the LJI team expanded ongoing immunoprofiling efforts for the first time to Zika-specific CD8 T cells. The isolation of Zika-specific T cells from the blood of previously infected individual had been made possible through earlier epitope identifications efforts funded through the NIH’s T cells Immune Epitope Discovery contracts.
Specifically, the researchers collected blood samples from convalescent Zika-infected donors in Puerto Rico and compared gene expression patterns between activated and inactivated CD8 T cells. “The gene expression profile revealed a fully functional T cell response that includes the capacity to kill infected cells and the secretion of cytokines answering the question whether the immune system can mount an effective CD8 T cell response to Zika,” says postdoctoral researcher and first author Alba Grifoni, Ph.D.
To confirm these results can be reproduced in an independent cohort, Grifoni analyzed samples from donors in Colombia between one and two years after they had been diagnosed with Zika. The researcher found the same characteristics she had observed shortly after the infection in the Puerto Rican cohort, “which means that what we see is not only stable over time but also over geographic distance,” says LJI Instructor Daniela Weiskopf, Ph.D., who coauthored the study. “This is really important because it underlines that our conclusions are broadly applicable.”
Since the samples were taken when the tested individuals had already recovered from their Zika infection, the measured immune response reflects at least to a certain degree the memory response, which is directly relevant to vaccination. “It informs what a protective immune response should look like and provides a baseline to establish the efficacy of vaccine candidates,” says Grifoni.
The work was funded by the National Institutes of Health through contracts HHSN272200900042C, HHSN27220140045C, HHSN268201100001I, grants U19 AI118626-01, S10OD016262, S10 RR027366 and S10OD016262. Further support was provided by the Zika Preparedness Latin American Network, which has received funding from the European Union’s Horizon 2020 research and innovation program under Grant Agreement 734584. Blood donor samples from Puerto Rico and Florida were collected as part of the National Heart, Lung, and Blood Institute Recipient Epidemiology and Donor Evaluation Study-III.
Full citation:
Alba Grifoni, Priscilla Costa-Ramos, John Pham, Yuan Tian, Sandy L. Rosales, Gregory Seumois, John Sidney, Aruna D. de Silva, Prem Lakshmanane, Matthew H. Collins, Mars Stone, Phillip J. Norris, Claudia M. E. Romero, Anna Durbin, Michael J. Ricciardi, Julie E. Ledgerwood, Aravinda M. de Silva, Michael Busch, Bjoern Peters, Pandurangan Vijayanand, Eva Harris, Andrew K. Falconar, Esper Kallas, Daniela Weiskopf, and Alessandro Sette. Transcriptional Profiling Reveals Multifunctional and Cytotoxic Antiviral Responses of Zika Virus–Specific CD8+ T Cells. Journal of Immunology, 2018. Doi: 10.4049/jimmunol.1801090
About La Jolla Institute for Immunology
The La Jolla Institute for Immunology is dedicated to understanding the intricacies and power of the immune system so that we may apply that knowledge to promote human health and prevent a wide range of diseases. Since its founding in 1988 as an independent, nonprofit research organization, the Institute has made numerous advances leading toward its goal: life without disease.
###


