Our Approach
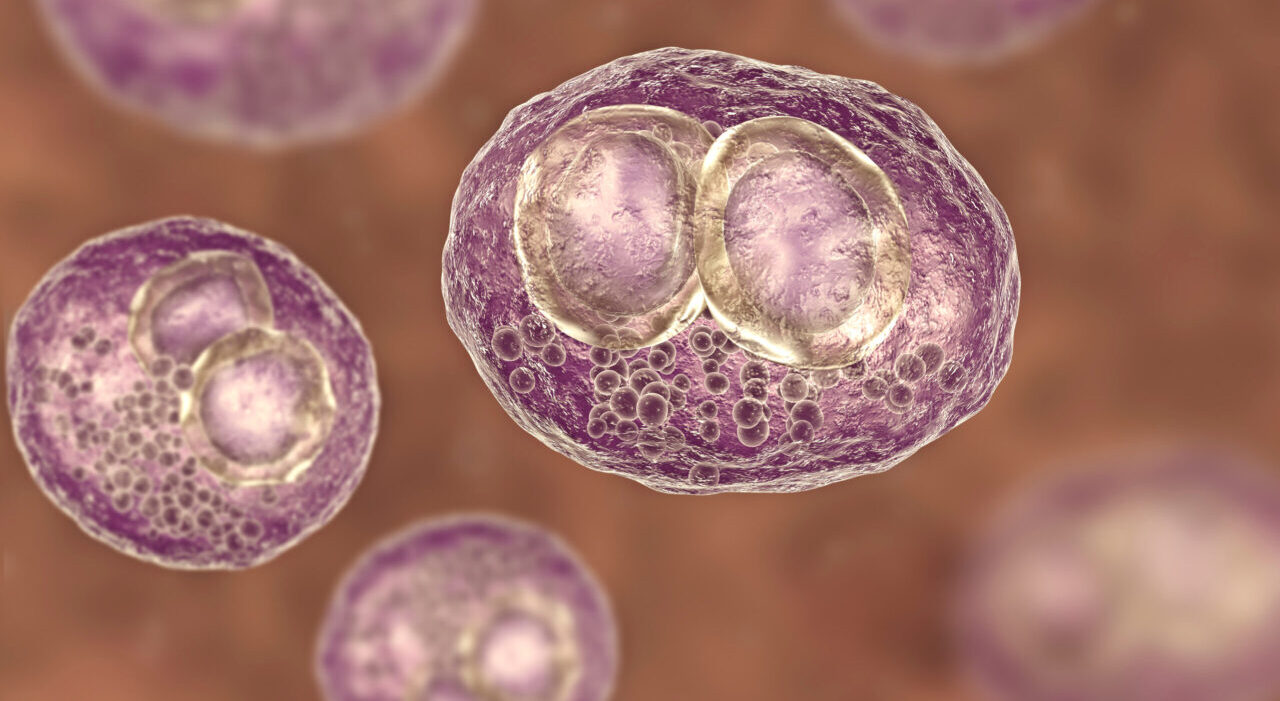
LJI scientists are working to define the molecular underpinnings of CMV infection in order to design effective vaccine strategies.
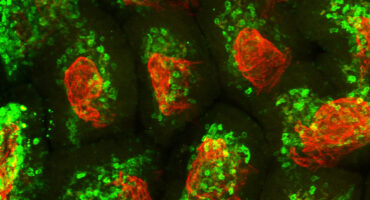
As a rapid response to infection, many cells display so-called “death receptors” that trigger cell death when activated by a cytokine called TRAIL. This “cell suicide” response helps clear out cells that could spread the virus. Several years ago, LJI Associate Professor Chris Benedict, Ph.D., discovered that CMV eludes that immune response by producing a protein called UL141, which jams those TRAIL signals. This uncanny ability to sabotage TRAIL signals explained how CMV-infected cells could survive and allow the infection to persist.
Very recently, Benedict identified a group of innate immune cells called ILC1s as the major cell type responsive to TRAIL signals. These cells are closely related to other innate immune cells named natural killer (NK) cells, which also mount an immediate response to some viral infections. Using mouse models, Benedict has discovered that it is ILC1s, not NK cells, that actually “contain” the CMV via unique mechanisms. Since ILC1s also exist in humans, this work furthers our understanding of how one might recruit these cells in an CMV vaccine.
Benedict has also identified unique CMV protein structures, or epitopes, recognized by T cells in both mice and man. One of these epitopes induces a unique ‘late rising’ T cell type that completely resolves CMV replication that can persist for many months. His lab found that vaccination with this and other epitopes elicits T cells that mediate dramatic protection in mice, indicating that it should also be possible to implement similar preventative approaches in humans.