LA JOLLA, CA—Allergic to peanuts? Bees? Pollen? Cockroaches? There’s a shot for that.
Each year, around 2.6 million Americans receive allergy immunotherapies, commonly called “allergy shots.” These therapies have been available for decades, and they are generally safe and effective.
Here’s the surprising part—scientists still don’t have a complete understanding of how allergy immunotherapies work. We know these therapies contain small amounts of an allergen. And we know this allergen exposure desensitizes immune cells and helps prevent allergic reactions.
Yet scientists don’t know how different doses of an allergen might affect different patients—and we don’t know which immune cells are the best targets for these therapies.
Now scientists at La Jolla Institute for Immunology (LJI) are investigating how allergy immunotherapies target the very immune cells that drive dangerous allergic reactions.
“The good thing is that allergy immunotherapies work,” says LJI Professor Alessandro Sette, Dr.Biol.Sci. “But we need to go deeper and characterize immune responses to allergen immunotherapies.”
Learning from cockroach allergies
Sette and his colleagues are uncovering the fundamentals of allergy immunotherapies by examining the immune system’s T cells in more detail than ever before. T cells are important because they drive allergic reactions. T cells “remember” past exposures to allergens, and they alert other immune cells when an allergen is present.
For a recent study in the Journal of Allergy and Clinical Immunology, the researchers focused on how allergy immunotherapies affected T cell responses in children (ages 8 to 17) with cockroach allergies.
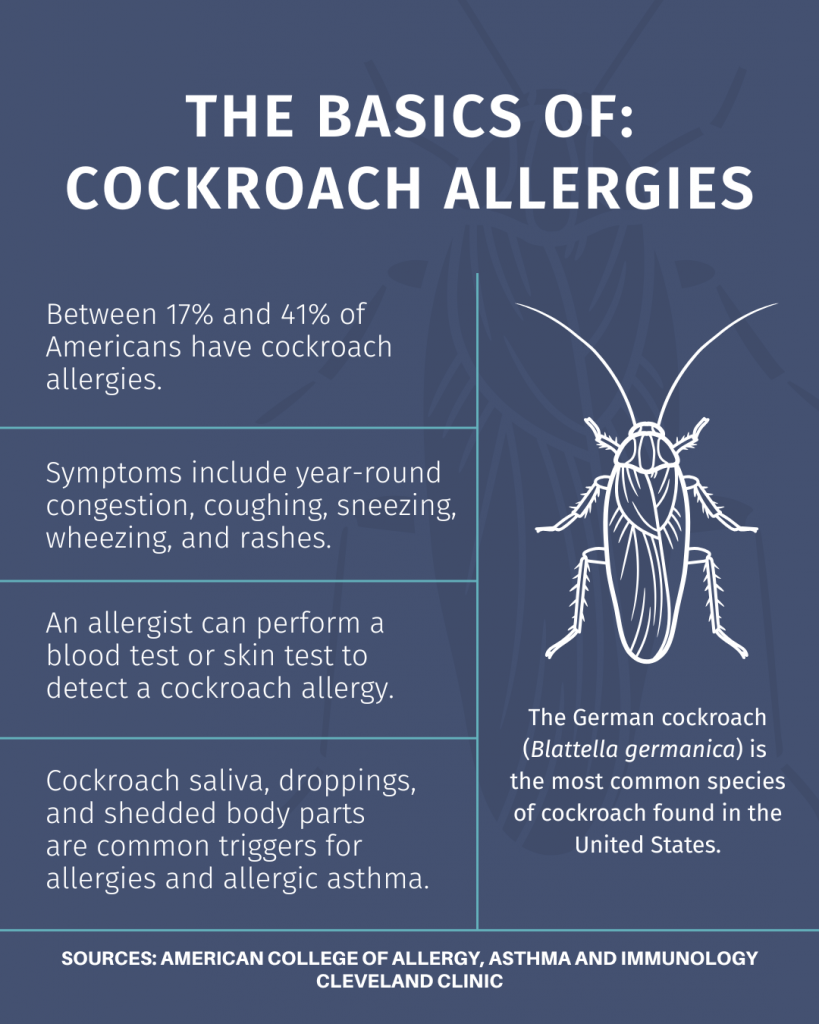
Cockroach allergies are extremely common, especially in urban and under-resourced areas, where around 89 percent of homes have detectable cockroach allergens. Young children are most likely to develop cockroach allergies—and most likely to experience potentially deadly allergic asthma attacks.
Like many children with cockroach allergies, the children in this study received allergy immunotherapy that contained cockroach “extract.” This extract includes proteins from cockroaches and cockroach droppings, which are processed and purified to be safe for injection.
But extracts are not all uniform. There are different ways to prepare allergen extracts, and some extracts contain more or less of the actual allergen. So does dosage make a difference?
The researchers found no difference in T cell responses to allergens present in high vs. low amounts in the extract. As long as you’re including the right cockroach proteins in an extract, the dosage doesn’t seem to matter. As Sette puts it, “A little goes a long way.”
“That’s good news. From one extract to the next, you can expect to get a more or less consistent immunological effect,” says Sette.
This research also helped the scientists zero in on a specialized type of T cells, called Th2 cells, as the main targets of allergy immunotherapy. “This type of T cell is important for the development of asthma and allergic reactions,” says Sette.
This finding helps explain why allergy immunotherapies tend to work so well. If you can desensitize Th2 cells to an allergen, you can likely dampen those harmful symptoms.
Stopping a “runaway train”
Next, the LJI team investigated how cockroach allergy immunotherapies worked in different groups of kids. They compared Th2 cell responses from kids who were highly allergic to cockroaches to kids who were weakly allergic to cockroaches. Which group might benefit more?
“Perhaps a cockroach extract would only work in someone highly allergic to cockroaches,” says Sette. “Because if you’re not highly allergic, maybe you don’t get as much benefit.”
Then again, says Sette, scientists have wondered if weak allergies are easier to control. “Perhaps if someone is strongly allergic, it’s more difficult to inhibit. It’s very hard to stop a runaway train going full speed,” says Sette.
The LJI experiments led to more good news. Sette and his colleagues found that cockroach allergy immunotherapies work no matter how strong a person’s underlying allergic response is.
Going forward, the researchers plan to broaden the research and investigate other T cell subtypes. They also plan to look at gene expression to better understand which T cells are targeted during allergy immunotherapy.
Understanding these fundamentals may reveal ways to tweak allergy immunotherapies to make them more effective for more patients. “This research may open the road to developing immunotherapies that aren’t based on crude extracts but are much more defined on a molecular level,” says LJI Senior Staff Scientist Ricardo Da Silva Antunes, Ph.D., who served as first author of the study.
Additional authors of the study, “Cockroach immunotherapy modulates dominant T cell responses independent of allergen extract content,” include Aaron Sutherland, Adam Abawi, April Frazier, Anna Pomés, Jill Glesner, Jay E. Slater, Samuel T. Mindaye, Kate Cho, Grace Zhou, Marie V. Ozanne, Agustin Calatroni, Cynthia M. Visness, Matthew C. Altman, Robert A. Wood, George T. O’Connor, Jacqueline A. Pongracic, Gurjit K. Khurana Hershey, Carolyn M. Kercsmar, Rebecca S. Gruchalla, Michelle Gill, Daniel Searing, Andrew H. Liu, Edward Zoratti, Meyer Kattan, Paula J. Busse, Will Sheehan, Leonard B. Bacharier, Stephen J. Teach, Lisa M. Wheatley, Alkis Togias, William W. Busse, Daniel J. Jackson.
This study was supported by the National Institutes of Health (NIH) National Institute of Allergy and Infectious Diseases (NIAID; grants 1UM1AI114271‐01, UM2AI117870, 5UM1AI114271‐03), the NIH’s National Center for Research Resources, and National Center for Advancing Translational Sciences (grants NCATS/NIH 64 UL1TR001079, NCATS/NIH UL1TR001422, NCATS/NIH UL1TR001876, NIH/CTSA 65 5UL1TR001425‐03, and NIAID/NIH U19AI135731.)