Center for Sex-based Differences in the Immune System
Disease affects men and women differently, and sex-specific health differences can be glaring. Women are better at fighting off infection but are more likely to develop an autoimmune condition, with 80 percent of autoimmune disease cases diagnosed in females. Men are more prone to heart disease and neurodegenerative diseases such as Parkinson’s. Some of these cases may come down to genetic differences that are the result of differential x-chromosome inactivation; sex hormone level; gender; behavior, or life experiences. But that is only part of the explanation.
“It’s become clear that sex-specific differences in the immune system are intimately tied to certain disease outcomes.”
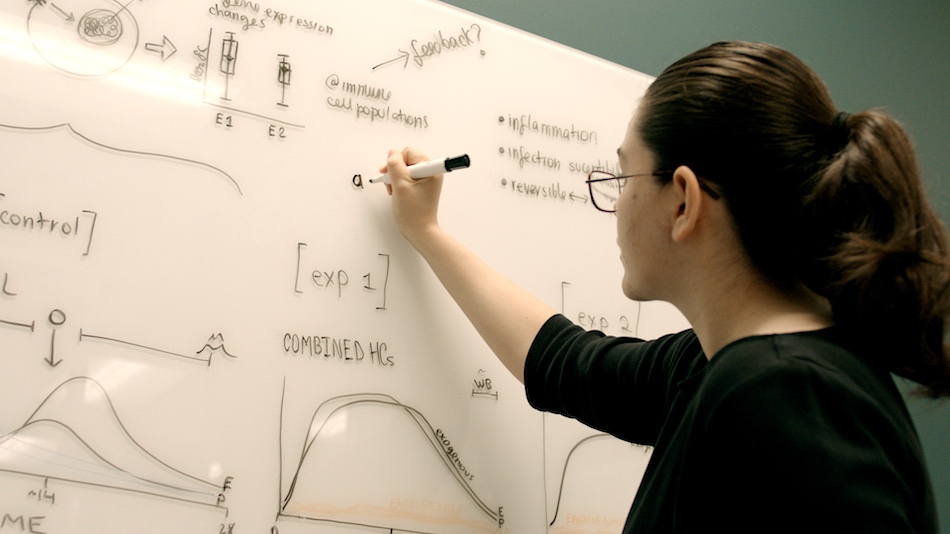
As part of LJI’s Sex-Based Differences in the Immune System Initiative, LJI scientists will bring the full breadth and depth of their expertise to understanding key differences between the immune responses in male and female individuals, down to individual immune cells.
“Studying sex-based differences in a systematic manner will help uncover the causes and allow for treatments that are in tune with biology.”
Our Approach
Immune Cell Profiling
Mapping and comparing the activity of dozens of different immune cells from thousands of individuals is something LJI researchers are known for worldwide. Professor Pandurangan Vijayanand, M.D., Ph.D., and his team discovered new genes in a CD4+ “helper” T cell subset that are linked to an increased risk in autoimmune disease. Intriguingly, they also uncovered major differences between individuals based on genetics and how these cells may function in men and women.
X chromosomes
Every female cell has two X chromosomes, one of which is shut down in female embryos during early development. The elaborate and tightly orchestrated process involves wrapping one of the X chromosomes into a highly compacted cocoon-like structure called heterochromatin. All chromosomes use heterochromatin to suppress “parasitic” DNA elements that have invaded the human genome. Professor Anjana Rao studies how problems with heterochromatin integrity can disturb the function of cells such as regulatory T cells, which use genes on the X-chromosome to prevent autoimmune and inflammatory diseases.
Big Data
To fuel further research into human immunity, the LJI team has created a free online resource for other immunologists around the world, the Database of Immune Cell Gene Expression, Expression of quantitative trait loci (eQTLs) and Epigenomics (DICE). DICE houses the massive data sets that result from immunoprofiling efforts that detail how variations in DNA sequence and sex-based differences impact gene activity in different types of immune cells.
Neurodegenerative Disease
Research Assistant Professor Cecilia Lindestam Arlehamn, Ph.D., is studying T cells to shed light on why men are more likely to develop Parkinson’s Disease. Working closely with Professor Alessandro Sette, Dr.Biol.Sci., she showed that autoreactive T cells can attack clumps of misfolded alpha-synuclein, the hallmark of Parkinson’s Disease. This T cell activity is a sign that Parkinson’s could be an autoimmune disease at its core. Dr. Lindestam Arlehamn is now following up on preliminary observations that the number of T cells and their reactivity differ in women and men. Associate Professor Sonia Sharma, Ph.D., is looking at sex-specific differences in early-onset dementia and Alzheimer’s and has already uncovered a specific group of bioactive lipids that show up in dramatically different numbers in men and women with Alzheimer’s.
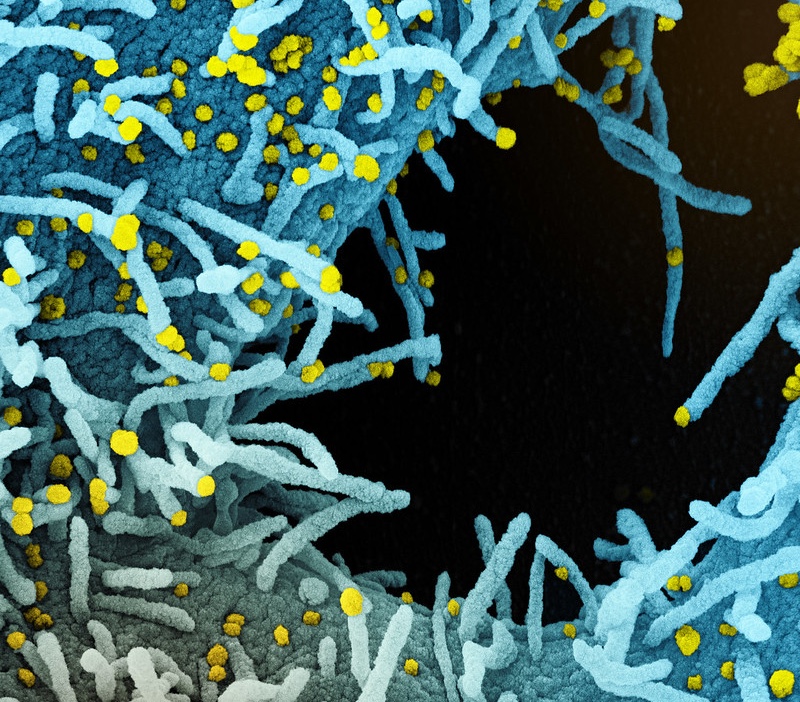
Infectious Disease
Men tend to be more susceptible to acute viral diseases and COVID-19 is no exception. Dr. Sette and Professor Shane Crotty, Ph.D., are looking for differences in immune responses to SARS-CoV-2 in women and men. Dr. Sharma is interested in the long-term inflammation affecting COVID-19 “long haulers.” The vascular inflammation and lingering multi-organ damage seen in COVID-19 cases is similar to vasculitis, an autoimmune disease that affects more women than men, and which Dr. Sharma studies.
Silent Viruses
Deep within our genomes are ancient “endogenous” retroviruses, DNA inserted from viral infections in our evolution. Usually these sequences are silent, but growing evidence now indicates that awakening of these genes and production of their products can be linked to autoimmune disease, breast and ovarian cancer. LJI President and CEO Erica Ollmann Saphire, Ph.D. is studying the structures of these ancient viral molecules and antibody responses against them which could provide new detection and treatment strategies.
Maternal Immune System
A pregnant woman’s immune system is intriguing because it interacts with an unusual, transient organ: the placenta. The placenta has strong defenses to keep pathogens from reaching the developing fetus. Zika virus is an exception. The virus can breach the placenta and cause severe neurodevelopmental problems. Professor Sujan Shresta, Ph.D., has published several studies showing how T cells in pregnant mice react to Zika—and how their young have fared. She also studies how CD8+ T cells that fight Zika in pregnant mice react to related viruses such as dengue.
Pregnancy is a critical time for viral infection. Associate Professor Chris Benedict, Ph.D., is studying immune responses against cytomegalovirus, which can cause devastating birth defects and Dr. Saphire is developing antibody treatments and vaccines for Lassa virus, which is up to 90% lethal in pregnant women.
“A better understanding of the placenta and the maternal immune system could shed light on a huge range of pregnancy complications and autoimmune diseases.”
Inflammatory Diseases
Dr. Sharma’s laboratory has uncovered a specific group of bioactive lipids that show up in dramatically different numbers in men and women with inflammatory diseases. These bioactive lipids, a unique and poorly understood class of signaling molecules, could fuel inflammation and explain sex-specific differences in how men and women develop heart disease, Alzheimer’s, COVID-19 or autoimmune vasculitis.
Autoimmune Diseases
The labs of Associate Professor Ferhat Ay, Ph.D., and Adjunct Professor Nunzio Bottini, M.D., Ph.D., identified a specific subset of T cells that were enriched in the joints of mice with rheumatoid arthritis (RA). They have characterized novel gene markers that contribute to the pathogenicity of this cell subset and discovered that cells expressing the same markers were present in the synovial biopsies of RA patients. Targeting these genes may lead to novel therapies for RA, a disease that is twice as common as well as more severe in women.
Labs
Selected Publications
- Cell Host Microbe
Related News
- Research News
- Immune Matters
- Immune Matters
- Immune Matters
- Immune Matters
- Immune Matters