Influenza
Influenza, or “the flu,” is a viral disease that causes symptoms such as fevers, coughing, congestion, sore throat, fatigue, and body aches. In severe cases, influenza can lead to hospitalization and even death. Infants, the elderly, and people with chronic health conditions, such as asthma or heart disease, are especially vulnerable to severe influenza. People with compromised immune systems, such as during cancer treatment or during pregnancy, are also at greater risk of severe disease.
Severe influenza can also lead to viral pneumonia, which causes lung tissues to swell and the lungs to fill with fluid. Together with pneumonia, influenza leads to around 35,000 to 45,000 deaths per year, according to the U.S. Centers for Disease Control and Prevention.
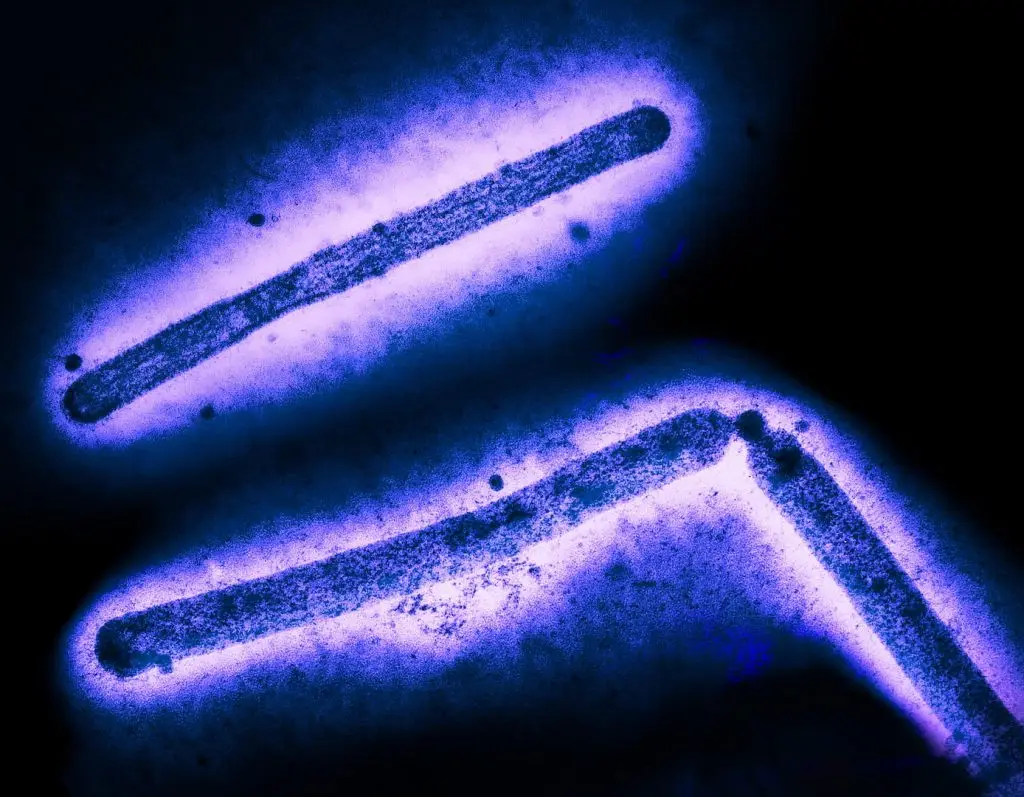
Influenza is caused by a family of respiratory viruses known as Orthomyxoviridae. This viral family is known for mutating quickly. Because influenza viruses are constantly mutating, experts recommend annual vaccines against the dominant influenza variants that circulate in any given year.
Some influenza viruses have pandemic potential. Many of these highly infective strains can be passed between humans and animal species, such as birds and swine. Notable strains of influenza include H1N1 (cause of the 1918-1920 Spanish flu pandemic), H1N1pdm09 (cause of the 2009 “swine flu” outbreak), and H5N1 (cause of the 2024-2025 cases of avian influenza).
Annual vaccines provide immunity against seasonal strains of influenza virus, but we don’t yet have a vaccine that offers durable protection against the overall family of influenza viruses.
Our Approach
Scientists at La Jolla Institute for Immunology (LJI) are investigating exactly how the human immune system combats different influenza viruses. Their research may guide the development of vaccines that spark a lasting and protective response against these deadly viruses.
Uncovering the importance of T cells
LJI Professor Alessandro Sette, Dr.Biol.Sci., and LJI Research Assistant Professor Alba Grifoni, Ph.D., have lead critical research into how the immune system’s T cells respond to H5N1, an influenza strain that caused causes of “bird flu” in 2024 and 2025.
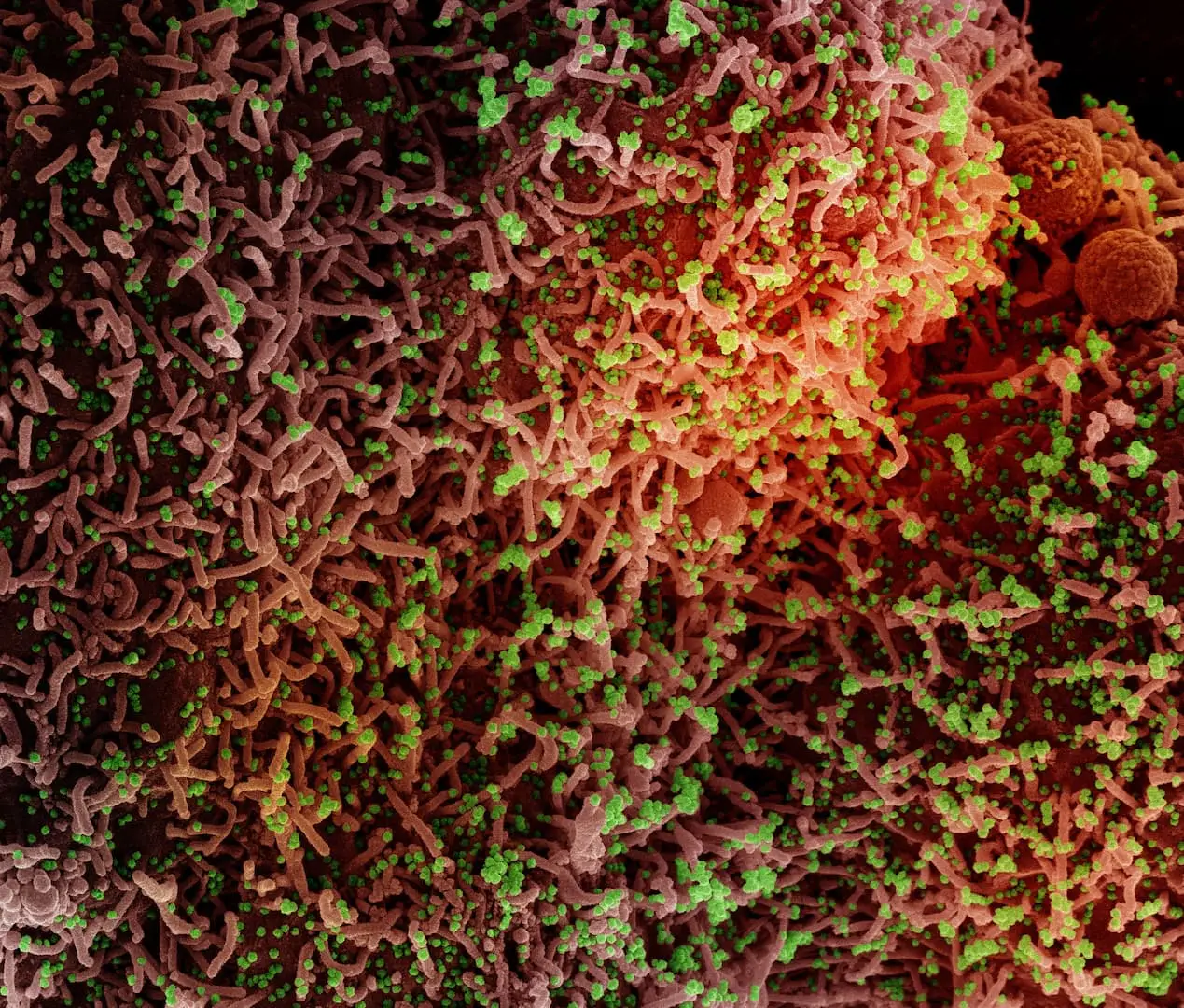
T cells are key players in viral immunity. These cells help eliminate infection cells, which stops a viral infection from spreading to additional healthy cells. T cells are also important because they alert antibody-producing B cells to danger.
Drs. Sette and Grifoni discovered that compared genetic sequences from H5N1 to genetic sequences from seasonal influenza viruses that already circulate in humans. The LJI team uncovered important similarities between H5N1 and these common viruses. People who have received seasonal flu vaccines or have had past cases of the flu have already built-up T cell protection against the more common flu viruses.
That T cell memory is important. The LJI scientists predicted that the family resemblance between influenza viruses may give “cross-reactive” T cells a head-start in recognizing H5NI infection and fighting back against severe disease.
By investigating how T cells respond to this ever-evolving family of viruses, Drs. Sette and Grifoni are helping to guide the development of vaccines that may prime T cells to protect against many influenza viruses at once.
Measuring antibodies to help at-risk patients
Research led by LJI Assistant Professor Tal Einav, Ph.D., is key to understanding why seasonal flu vaccines protect some people more than others. What is the difference between “strong” vaccine responders and “weak” vaccine responders?
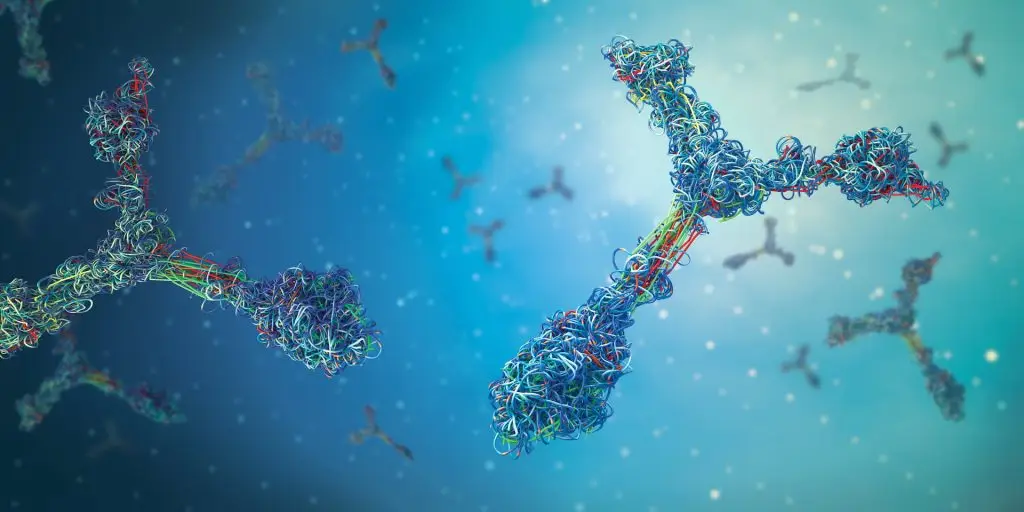
Dr. Einav is taking a closer look at immune system memory. When a person gets a vaccine or experiences a viral infection, their body churns out specialized immune cells and antibodies. Some of those immune cells and antibodies stick around for years to provide long-term protection against disease.
Scientists can measure the strength of this immune system “memory” by examining antibody levels, or titers, in a person’s blood. Antibody titers act as a sort of historical record of what your immune system has encountered during your life.
In a recent study, Dr. Einav developed AI tools to analyze antibody responses from thousands of people who received seasonal flu vaccines. His study showed that the best way to predict a person’s response to an upcoming flu vaccine (containing the currently circulating flu strain) is to measure their immune response to the flu vaccine strain used the year before—and the year before that—and the year before that.
In fact, a person’s responses to prior flu strains is an even better predictor of future responses than a person’s age, sex, geographic location, or the vaccine dose they receive.
Dr. Einav and his colleagues are now looking for immune system markers that might show whether certain vaccine formulations can boost immune cell reactions in weak responders. This work is an important step toward more personalized and effective vaccines.
Learn More:
Related News
- Research News
- Research News