LA JOLLA, CA—A big question on people’s minds these days: how long does immunity to SARS-CoV-2 last following infection?
Now a research team from La Jolla Institute for Immunology (LJI), The University of Liverpool and the University of Southampton has uncovered an interesting clue. Their new study suggests that people with severe COVID-19 cases may be left with more of the protective “memory” T cells needed to fight reinfection.
“The data from this study suggest people with severe COVID-19 cases may have stronger long-term immunity,” says study co-leader LJI Professor Pandurangan Vijayanand, M.D., Ph.D.
The research, published Jan. 21 in Science Immunology, is the first to describe the T cells that fight SARS-CoV-2 in “high resolution” detail.
“This study highlights the enormous variability in how human beings react to a viral challenge,” adds co-leader Christian H Ottensmeier, M.D., Ph.D., FRCP, a professor at the University of Liverpool and adjunct professor at LJI.
Since early in the COVID-19 pandemic, scientists at LJI have investigated which antibodies and T cells are important for fighting SARS-CoV-2. As experts in genomics, Vijayanand and Ottensmeier have used sequencing tools to uncover which T cell subsets may control disease severity. In October, the team published the first detailed look at how CD4+ T cells respond to the virus.
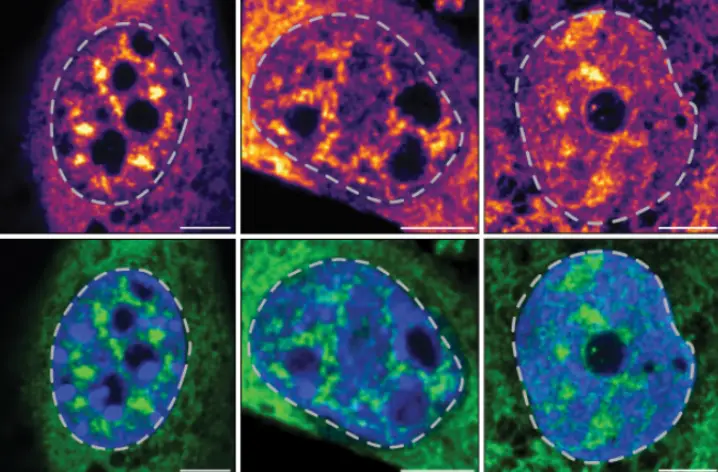
For the new study, the researchers used a technique called single-cell transcriptomics analysis to study the expression of individual genes of more than 80,000 CD8+ T cells isolated from both COVID-19 patients and non-exposed donors. CD8+ T cells are the cells responsible for destroying virus-infected host cells. “Memory” CD8+ T cells are also important for protecting the body from reinfection against many viruses.
The team studied CD8+ T cells from 39 COVID-19 patients and 10 subjects who had never been exposed to the virus (their blood samples were given before the pandemic). Of the COVID-19 patients, 17 patients had a milder case that did not require hospitalization, 13 had been hospitalized, and nine had needed additional ICU support.

To the researchers’ surprise, they saw weaker CD8+ T cell responses in patients with milder COVID-19 cases. The researchers saw the strongest CD8+ T cell responses in the severely ill patients who required hospitalization or ICU support.
“There is an inverse link between how poorly T cells work and how bad the infection is,” says Ottensmeier. “I think that was quite unexpected.”
One could expect to see a stronger CD8+ T cell response in the mild cases, since these are the cases where the immune system was equipped to fight off a severe infection—but the study showed the opposite. In fact, CD8+ T cells in the milder cases showed the molecular signs of a phenomenon called T cell “exhaustion.” In cases of T cell exhaustion, cells receive so much immune system stimulation during a viral attack that they are less effective in doing their jobs.
While more research is needed, Vijayanand and Ottensmeier think it is worth studying whether T cell exhaustion in the mild COVID-19 cases may hinder a person’s ability to build long-term immunity.
“People who have severe disease are likely to end up with a good number of memory cells,” says Vijayanand. “People with milder disease have memory cells, but they seem exhausted and dysfunctional—so they might not be effective for long enough.”
The new study provides a valuable window into CD8+ T cell responses, but it is limited because it relies on the CD8+ T cells found in blood samples. As a next step, the researchers hope to shed light on how T cells in tissues hit hardest by SARS-CoV-2, such as the lungs, react to the virus. This step will be important because the memory T cells that provide long-term immunity need to live in the tissues.
“This study is very much a first step in understanding the spectrum of immune responses against infectious agents,” says Ottensmeier. Going forward, the researchers hope to use single-cell sequencing techniques to look at CD8+ T cells in cancer patients with COVID-19 infection.
“This research highlights the power of these new tools to understand human immunology,” says Vijayanand.
The new study, titled “Severely ill COVID-19 patients display impaired exhaustion features in SARS-CoV-2-reactive CD8+ T cells,” was supported by the National Institutes of Health (grants U19AI142742, U19AI118626, R01HL114093, R35-GM128938, S10RR027366, S10OD025052, the William K. Bowes Jr Foundation, the Whittaker Foundation, the Wessex Clinical Research Network and the National Institute of Health Research UK.
Additional study authors include co-first authors Anthony Kusnadi, Ciro Ramírez-Suástegui, Vicente Fajardo and Serena J Chee, as well as Benjamin J Meckiff, Hayley Simon, Emanuela Pelosi, Grégory Seumois and Ferhat Ay.
DOI: 10.1126/sciimmunol.abe4782
###