LA JOLLA, CA—Flu shots save lives across the United States every year. These vaccines are good at protecting the population from severe influenza infections, but not every person gets the same level of protection.
“Some people have incredibly strong responses to annual flu vaccines, and some people don’t respond at all,” says Tal Einav, Ph.D., Bodman Family Assistant Professor at La Jolla Institute for Immunology (LJI) and member of LJI’s Center for Vaccine Innovation.
Einav and his colleagues have developed a machine learning model to analyze massive datasets from multiple flu vaccine studies. The researchers are using this tool to solve a big mystery in science: Can we predict who will be a weak vaccine responder or a strong vaccine responder?
The research team shared their findings in a recent eBioMedicine study. They used their machine learning model to spot trends across 20,000 antibody responses from influenza studies conducted between 1997 and 2021. “From this vantage, with all these datasets, you can start to explore the vaccine response in fundamentally new ways,” says Einav, who served as study senior author.
The researchers discovered that the best way to predict a person’s response to an upcoming flu vaccine (containing the currently circulating flu strain) is to measure their immune response to the flu vaccine strain used the year before—and the year before that—and the year before that.
In fact, a person’s responses to prior flu strains is an even better predictor of future responses than a person’s age, sex, geographic location, or the vaccine dose they receive.
“Many studies have shown that age has an effect. We have just shown that it is a very small effect, whereas you can get far better predictions with antibody responses that can be measured from your blood,” says Einav.
Your blood remembers
The influenza virus acquires a few mutations each year, so researchers don’t tend to dwell on a person’s antibody response to past flu strains. Instead, researchers consider the response to the currently circulating strains.
The new LJI study shows the importance of looking back in time.
When a person gets a vaccine or experiences a viral infection, their body churns out specialized immune cells and antibodies. Some of those immune cells and antibodies stick around for years to provide long-term protection against disease.
Scientists can measure the strength of this immune system “memory” by examining antibody levels, or titers, in a person’s blood. Antibody titers are fascinating because they act as a sort of historical record of what your immune system has encountered during your life.
Because influenza mutates quickly—and flu vaccine formulations change each year—scientists can distinguish between your antibody response to viruses from this year, last year, or even earlier. By measuring all of these strains, researchers can assemble a reliable, chronological record of a person’s immune responses to the flu from each year.
“Blood doesn’t forget,” says Einav.
The “signature” of a strong vaccine responder
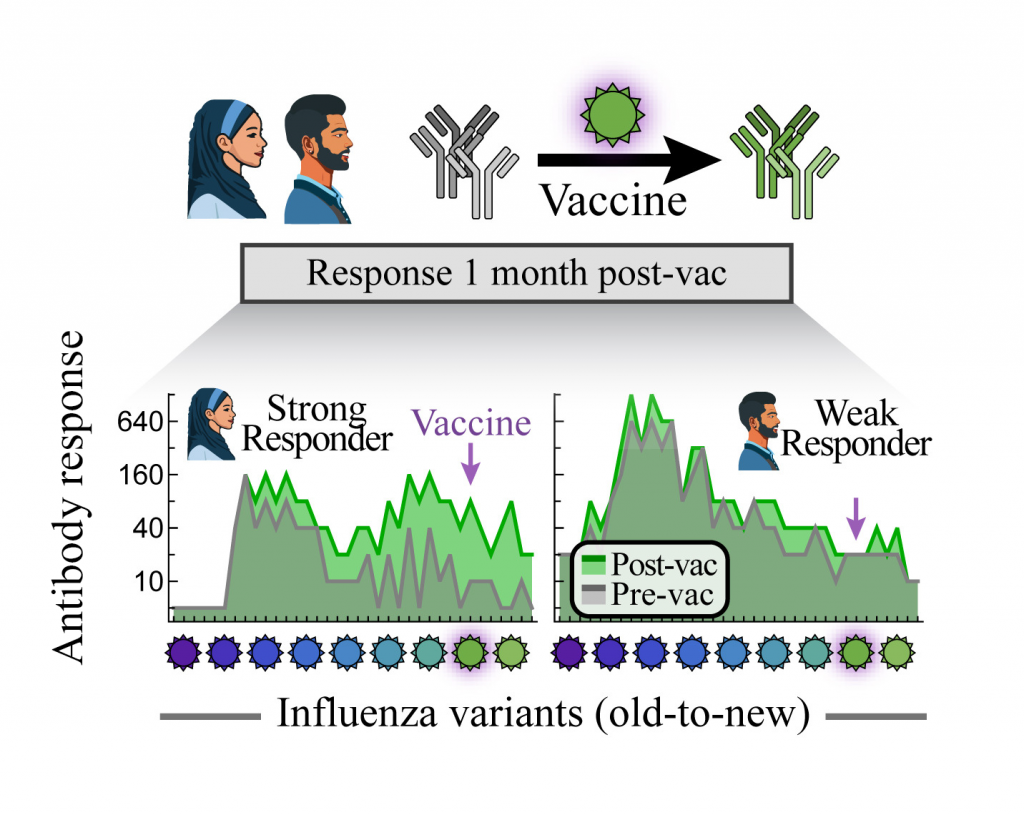
The left side shows antibody responses from a strong vaccine responder. This strong responder has antibody titers with “jagged” fluctuations in response to different influenza virus variants through the years.
The right side shows a typical signature of a weak vaccine responder. This responder still has some response to influenza virus variants, but the overall response decreases through the years.
The researchers found that strong vaccine responders had “jagged” antibody titers that would be high in one year, low against the prior year’s strain, high again the year before that, and continue in this fashion. On a timeline, these peaks create a regular pattern that resembles a row of shark teeth, where each peak indicates a strong response to that specific flu strain.
Einav says these yearly fluctuations are a useful “signature” of an immune system on high alert. “Strong responders tended to have these jagged peaks,” says Einav.
Antibody titers looked quite different in weak responders, whose timeline plots tended to be smoother. Some weak responders had antibody responses that more frequently plateaued across years. Their antibody response against this year’s flu strain tends to be similar to their response to next year’s strain. “Yet when the virus evolves the next year, and the vaccine changes, these individuals tend to respond poorly,” says Einav.
While these results held across over 20 influenza seasons, the researchers further tested their machine learning model on four recent vaccine studies they conducted in 2022 and 2023. These studies included data from a wide swath of study participants in La Jolla, CA, as well as in Athens, GA, who were given one of three influenza vaccine types.
The model held true. It didn’t matter what a person’s demographics were, or their vaccine type, their antibody response to current and past flu strains was the best predictor of whether they would be weak or strong responders.
What this means for yearly flu shots
Now LJI researchers are wondering: How can we help the weak responders?
“There are multiple different types of flu vaccines that you can get,” says Einav. “We want to know if people might respond better or worse if you give them a different vaccine formulation.”
Einav and his colleagues are now looking for immune system markers that might show whether certain vaccine formulations can boost immune cell reactions in weak responders. This work is an important step toward more personalized and effective vaccines.
“Our hope is to be able to predict for each person what their response is going to be for each different vaccine,” says Einav.
Moreover, Einav adds that this study was possible thanks to the multiple research groups from across the country sharing their data. “There are very generous researchers out there, and I really commend their efforts. We all want for our hard-won data to help make things better for all of us, and that is exactly what we do when we post our data,” says Einav. “We cannot even imagine the discoveries and applications that groups will achieve in the coming years using these datasets.”
Additional authors of the study, “Leveraging Pre-Vaccination Antibody Titers across Multiple Influenza H3N2 Variants to Forecast the Post-Vaccination Response,” included Hannah Stacey, Michael A. Carlock, James D. Allen, Hannah B. Hanley, Shane Crotty, and Ted M. Ross.
This research was supported by the University of California San Diego PREPARE Institute, LJI & Kyowa Kirin, Inc. (KKNA, Kyowa Kirin North America), the Bodman Family, the National Center for Advancing Translational Sciences of the NIH (CTRU, Award #UL1TR002378), Collaborative Influenza Vaccine Innovations Centers (CIVICs) of NIAID (Contract 1015 #75N93019C00052), University of Georgia, Cleveland Clinic, and by the Georgia Research Alliance (Georgia Eminent Scholar GRA-001).