LA JOLLA, CA—Scientists at La Jolla Institute for Immunology (LJI) have found that four COVID-19 vaccines (Pfizer-BioNTech, Moderna, J&J/Janssen, and Novavax) prompt the body to make effective, long-lasting T cells against SARS-CoV-2. These T cells can recognize SARS-CoV-2 Variants of Concern, including Delta and Omicron.
“The vast majority of T cell responses are still effective against Omicron,” says LJI Professor and study co-leader Alessandro Sette, Dr. Biol.Sci.
“These cells won’t stop you from getting infected, but in many cases they are likely to keep you from getting very ill,” adds LJI Professor Shane Crotty, Ph.D.
“And this is true in all the type of vaccines we studied—and up to six months after vaccination,” says LJI Instructor Alba Grifoni, Ph.D., who co-led the work with Sette and Crotty.
These data come from adults who were fully vaccinated, but not yet boosted. The researchers are now investigating T cell responses in boosted individuals and people who have experienced “breakthrough” COVID-19 cases.
The new Cell study also shows that fully vaccinated people have fewer memory B cells and neutralizing antibodies against the Omicron variant. This finding is in line with initial reports of waning immunity from laboratories around the world.
Without enough neutralizing antibodies, Omicron is more likely to cause a breakthrough infection. Fewer memory B cells means the body will then be slower to churn out additional neutralizing antibodies to fight the virus.
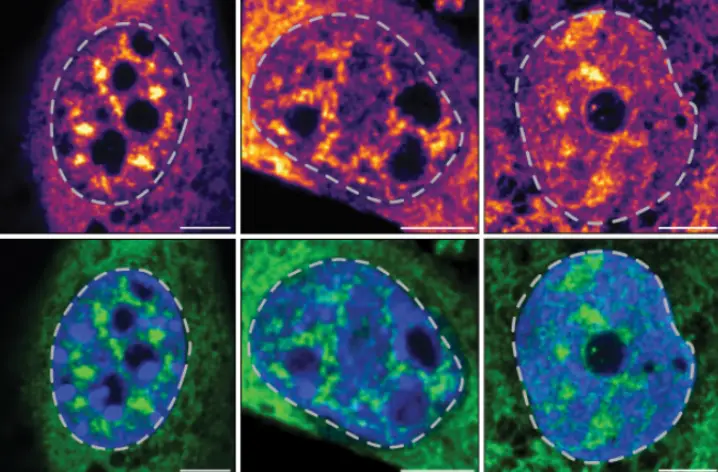
“Most of the neutralizing antibodies, i.e., the antibodies that work well against SARS-CoV-2, bind to a region called the receptor binding domain, or RBD,” says LJI Instructor Camila Coelho, Ph.D., who served as co-first author of the study. “Our study revealed that the 15 mutations present in Omicron RBD can considerably reduce the binding capacity of memory B cells, compared to other SARS-CoV-2 variants such as Alpha, Beta and Delta.”
How T cells fight Omicron
The good news is that neutralizing antibodies and memory B cells are just two arms of the body’s adaptive immune response. In a person exposed to SARS-CoV-2, T cells do not prevent infection. Instead, T cells patrol the body and destroy cells that are already infected, which prevents a virus from multiplying and causing severe disease.
The LJI team believes the “second line of defense” from T cells helps explain why Omicron infections are less likely to lead to severe disease in fully vaccinated people. (The variant is also appears to infect different tissues)
To know whether the vaccine-induced T cells they detected in their study were actually effective against variants such as Delta and Omicron, the scientists took a close look at how the T cells responded to different viral “epitopes.”
Every virus is made up of proteins that form a certain shape or architecture. A viral epitope is a specific landmark on this architecture that T cells have been trained to recognize. The current COVID-19 vaccines were designed to teach the immune system to recognize specific epitopes on the initial “Alpha” variant of SARS-CoV-2. As the virus has mutated, its architecture has changed, and the concern is that immune cells will no longer recognize their targets.
The new study shows that while the architecture of Omicron is different enough to evade some neutralizing antibodies and memory B cells, memory T cells still do a good job of recognizing their targets, even on the highly mutated Omicron variant. Overall, at least 83 percent of the CD4+ (helper) T cell responses and 85 percent of the CD8+ T cell responses stayed the same, no matter the vaccine or the variant.
Crotty notes that the memory B cells that do bind Omicron are likely to also contribute to protection against severe disease. “Vaccinated people have memory CD4+ T cells, CD8+ T cells, and memory B cells to help fight the infection if the virus gets past the initial antibodies, and having multiple lines of defense is likely an important strength,” Crotty says.
Omicron is still a threat
The researchers emphasize that no one should count on T cell protection alone. The LJI study sheds light on immunity at the population level, but individual immune responses vary, and relying on one’s untested immune system to fight COVID is a roll of the dice.
“I’d urge people to still be cautious and keep wearing masks,” says Alison Tarke, a graduate student and member of the Sette Lab who served as co-first author with Coelho. “There is a chance you are one of the few people with a declining immune response.”
“This work also emphasizes the importance of getting a booster,” adds Sette. (Find a booster near you)
The Sette and Crotty Labs have teamed up on COVID-19 research since early 2020. With the Sette Lab’s expertise in T cells and the Crotty Lab’s expertise in vaccine design and B cell responses, the collaboration has led to key insights into pre-existing SARS-CoV-2 immunity, vaccine responses, severe COVID cases and more.
Grifoni says the researchers are now looking at two pressing questions. First, they’d like to see what T cells, B cells and antibody responses look like after COVID-19 booster shots. Second, they are investigating what the immune response looks like after a breakthrough infection. (Volunteer for an LJI Clinical Study)
Additional authors of the study, “SARS-CoV-2 vaccination induces immunological memory able to cross-recognize variants from Alpha to Omicron,” are co-first author Zeli Zhang, co-first author Jennifer M. Dan, Esther Dawen Yu, Nils Methot, Nathaniel I. Bloom, Benjamin Goodwin, Elizabeth Phillips, Simon Mallal, John Sidney, Gilberto Filaci, Daniela Weiskopf and Ricardo da Silva Antunes.
This research was supported by the National Institutes of Health’s National Institute of of Allergy and Infectious Diseases (contracts No. 75N93021C00016 to A.S. and 75N9301900065) and a PhD student fellowship through the Clinical and Experimental Immunology Course at the University of Genoa, Italy