LA JOLLA, CA—Researchers at La Jolla Institute for Immunology (LJI) have found that Zika virus can mutate to become more infective—and potentially break through pre-existing immunity.
“The world should monitor the emergence of this Zika virus variant,” says LJI Professor Sujan Shresta, Ph.D., who co-led the Cell Reports study with Professor Pei-Yong Shi, Ph.D., of the University of Texas Medical Branch (UTMB).
Zika virus is carried by mosquitoes, and the symptoms of Zika infection are usually mild in adults. However, the virus can infect a developing fetus, resulting in birth defects such as microcephaly.
Zika virus and dengue virus overlap in many countries worldwide. Like Zika, dengue virus is a mosquito-borne flavivirus, and thus shares many biological properties. In fact, the viruses are similar enough that the immune response sparked by prior dengue exposure can offer protection against Zika.
“In areas where Zika is prevalent, a vast majority of people have already been exposed to dengue virus and have both T cells and antibodies that cross-react,” says Shresta.
Unfortunately, both viruses are also quick to mutate. “Dengue and Zika are RNA viruses, which means they can change their genome,” explains Shresta. “When there are so many mosquitoes and so many human hosts, these viruses are constantly moving back and forth and evolving.”
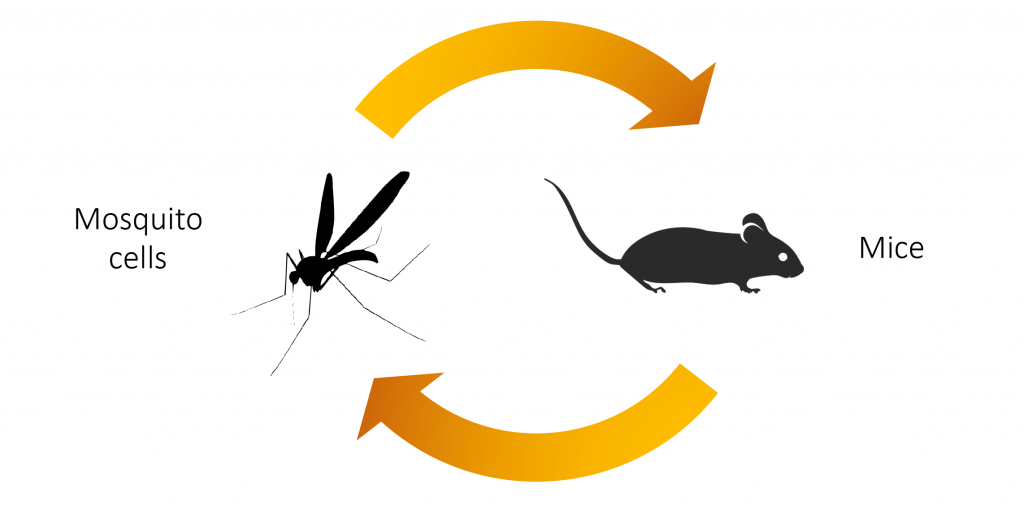
To study Zika’s fast-paced evolution, the LJI team recreated infection cycles that repeatedly switched back and forth between mosquito cells and mice. This work gave the LJI scientists a window into how Zika virus naturally evolves as it encounters more hosts.
The researchers found it is relatively easy for Zika virus to acquire a single amino acid change that allows the virus to make more copies of itself—and help infections take hold more easily. This mutation (called NS2B I39V/I39T mutation) boosts the virus’s ability to replicate in both mice and mosquitoes. This Zika variant also showed increased replication in human cells.
“This single mutation is sufficient to enhance Zika virus virulence,” says study first author Jose Angel Regla-Nava, Ph.D., former postdoctoral researcher at LJI and current Associate Professor at the University of Guadalajara, Mexico. “A high replication rate in either a mosquito or human host could increase viral transmission or pathogenicity—and cause a new outbreak.”
Adds Shresta, “The Zika variant that we identified had evolved to the point where the cross-protective immunity afforded by prior dengue infection was no longer effective in mice. Unfortunately for us, if this variant becomes prevalent, we may have the same issues in real life.”
So how can we prepare for this kind of variant? Shresta’s laboratory is already looking at ways to tailor Zika vaccines and treatments that counteract this dangerous mutation. She will also continue to work closely with Regla-Nava to better understand exactly how this mutation helps Zika replicate more efficiently.
“We want to understand at what point in the viral life cycle this mutation makes a difference,” says Shresta.
Additional authors of the study, “A Zika Virus Mutation Enhances Transmission Potential and Confers Escape from Protective Dengue Virus Immunity,” include first author Jose Angel Regla-Nava, Ying-Ting Wang, Camila R Fontes-Garfias, Yang Liu, Thasneem Syed, Mercylia Susantono, Andrew Gonzalez, Karla Viramontes, Shailendra Verma, Kenneth Kim, Sara Landeras-Bueno, Chun-Teng Huang, Daniil M Prigozhin, Joseph G Gleeson, and Alexey V Terskikh.
This research was supported by the National Institutes of Health (R01 AI153500, R01 AI163188, R56 AI148635, U01 AI151810, R01 NS106387, R01 AI134907, R43 AI145617, and UL1 TR001439), the Sealy & Smith Foundation, the Kleberg Foundation, the John S. Dunn Foundation, the Amon G. Carter Foundation, the Gilson Longenbaugh Foundation, and the Summerfield Robert Foundation.
DOI: 10.1016/j.celrep.2022.110655
###



