Seasonal Allergies
Almost 20 percent of the general population suffers seasonal allergies from springtime pollen exposure. One grass producing those allergens is called Timothy grass, grown in lawns and as animal forage throughout the U.S. and Europe. Timothy grass allergens evoke the familiar constellation of cough, runny nose, and itchy eyes in sensitized individuals, symptoms sometimes alleviated by anti-histaminic drugs or nasal sprays.
For those severely affected, so-called “allergy shots ” consisting of increasing doses of crude extracts made from Timothy grass pollen—a procedure known as allergen immunotherapy—provides the only long-lasting relief. This approach often succeeds in reprogramming the immune system to tolerate grass pollens; however, in rare cases, allergic immunotherapy can trigger anaphylactic shock and therefore is usually not even attempted in people who already have severe allergic asthma.
Our Approach
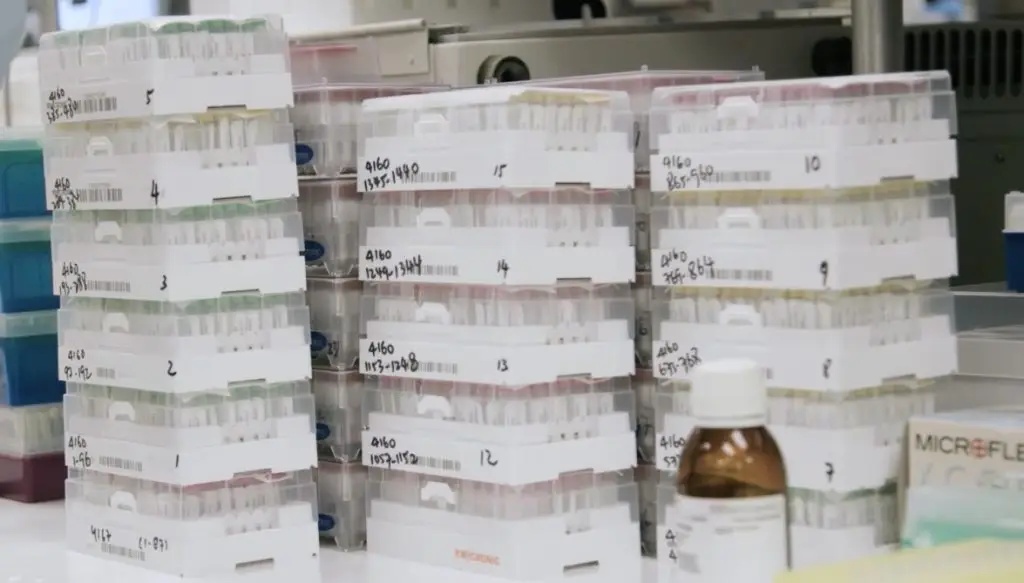
LJI researchers in the labs of Alessandro Sette, Ph.D., and Bjoern Peters, Ph.D., are assessing whether standard immunotherapies could be modified to minimize hypersensitivity. To do so, they are dissecting cellular responses to discrete components of Timothy grass extracts by analyzing immune cells in blood samples from patients inoculated with Timothy grass extracts. Previously, scientists knew that exposure to the entire extract stimulated B cells to produce an allergen-specific antibody called IgE, kicking off a cell- signaling cascade promoting an adverse allergic response.
The team has identified discrete protein fragments, or peptides, contained in Timothy grass extracts that activate an allergic response by stimulating T helper cells called Th2 cells without prompting B cells to generate high levels of IgE. Furthermore, these inflammatory Th2 responses appear to decrease with repeated immunotherapy, most significantly in patients who also report alleviation of symptoms.
This was a very positive sign, as an overly enthusiastic Th2 cell response underlies development of allergy and asthma in numerous contexts. Drs. Sette and Peters went on to asking whether immunotherapy with purified peptide cockroach allergens might be more effective in maintaining a healthy ratio of Th1 to Th2 cells.
In 2025, Dr. Sette published a closer look at how allergy immunotherapy affects T cell responses in children with cockroach allergies. Among his findings was the surprising discovery that allergen dosage doesn’t influence T cell response. As long as you’re including the right cockroach proteins in an extract, the dosage doesn’t seem to matter.
Still, LJI scientists want to find ways to make allergy immunotherapies even more effective. Dr. Sette plans to investigate gene expression in different T cell subtypes to better understand which T cells are targeted during this treatment.
Related News
- Research News