Dengue
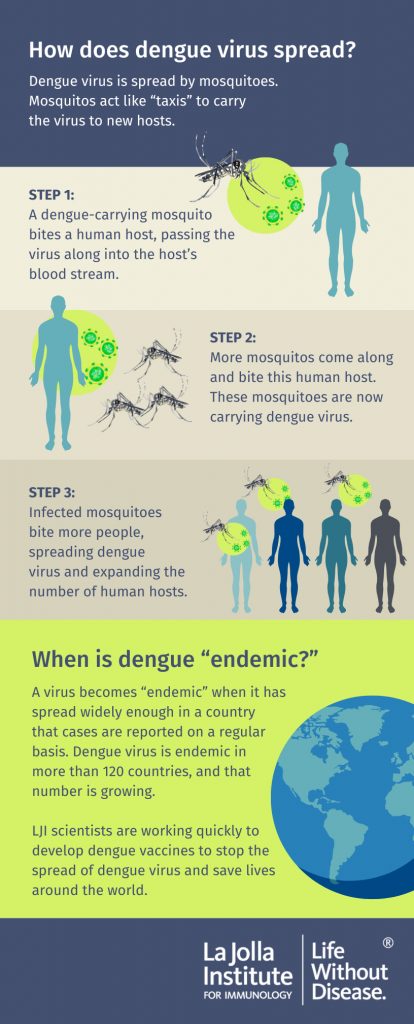
Dengue fever is a mosquito-borne disease caused by a type of flavivirus. The virus is closely related to the mosquito-borne Zika virus. Dengue infection is most common in tropical regions of Africa, Latin America and Asia, where genus Aedes mosquitoes spread the virus.
Most cases in the United States are brought in by travelers; however, San Diego and Los Angeles counties recently reported their first-ever cases of locally acquired dengue fever, raising the possibility that dengue virus may become endemic in the region.
Most people infected with dengue experience no symptoms or just mild flu-like symptoms. But of the nearly 400 million persons infected yearly, approximately 22,000 will die of lethal dengue hemorrhagic fever (DHF) or of blood pressure fluctuation known as dengue shock syndrome (DSS). Thus there is a pressing need to define molecular and cellular factors that govern why the disease progresses to a fatal form in some individuals. Equally critical is a need for effective prevention, as a current dengue vaccine is only marginally effective.
LJI scientists are working quickly to develop life-saving dengue vaccines. These experts are combining molecular and epidemiological approaches to better prevent infection and to treat severe dengue cases.
Our Approach
LJI scientists are advancing dengue vaccine research and uncovering the critical the role of T cell in fighting infection.
What makes dengue infection turn deadly?
To address why dengue infection only occasionally becomes lethal, LJI immunologists Alessandro Sette, Dr. Biol. Sci., and Bjoern Peters, Ph.D., performed “transcriptomic” comparisons of gene expression in immune cells taken from patients with either the mild or hemorrhagic forms of dengue as part of the Human Immunology Project Consortium. Their findings challenge a misconception, namely that the disease becomes lethal once a population of CD4-positive T cells, called “T helpers,” elicits an uncontrolled inflammatory response. Instead, the team observed little difference in number or gene expression pattern of CD4-positive T helpers in blood from either set of patients, suggesting that these cells respond to infection but do not behave differently in benign versus fatal forms of disease.
Other work from Dr. Sette’s lab complements these findings. His team has reported that a different type of T cell, CD8-positive “memory T cells,” mobilize after dengue infection and “remember” the virus, likely protecting individuals from severe disease.
Designing Better Vaccines
LJI Professor Sujan Shresta, Ph.D., constructs mouse models to study infection by both dengue and Zika. Mosquitoes that carry both viruses are present in geographically-overlapping regions; thus it is likely that people living in these regions will encounter both viruses in their lifetime. So it makes sense to have pan-flavivirus vaccines that target multiple flaviviruses.
In 2024, Dr. Shresta received substantial funding through the National Institute for Allergy and Infectious Diseases’ (NIAID) Flavivirus and Alphavirus ReVAMPP (FLARE) program to test dengue vaccines. Her laboratory is working with scientists nationwide to test experimental vaccine strategies against deadly viruses from the flavivirus and alphavirus families, including dengue virus and chikungunya.
Why study many flaviviruses at once?
Dr. Shresta and her colleagues have found that pre-existing immunity to one flavivirus can mediate both protection against another flavivirus—or it can lead to more severe infection, depending on the infection scenario. In fact, Dr. Shresta’s lab has found that which virus a person encounters first makes a difference in protection versus pathogenesis, as does the length of time between infections.
To better understand this phenomenon, Dr. Shresta uses mouse models to study immunological cross-reactivity between flaviviruses.
As an illustration, when Dr. Shresta infected mice first with dengue virus and then challenged these mice shortly after with Zika virus, the mice remained healthy; in contrast, mice with no prior exposure to dengue virus succumbed to Zika infection. This protective effect of prior dengue immunity was mediated by cross-reactive T cells that recognized both viruses. As another example, when Dr. Shresta exposed mouse pups born to Zika-immune mothers to dengue virus, all pups died of lethal dengue disease—an outcome not seen in pups with no Zika immunity. This hyper-lethality occurred because transfer of anti-Zika antibodies from the mother to her offspring made them unusually vulnerable to dengue infection.
The lab continues to dissect the interplay between the cross-reactive T cell and antibody responses to these viruses and trying to understand the rules that govern when they are good and when they are bad. Dr. Shresta’s goal is to harness the good effects of cross-reactivity and avoid the bad to develop safe, effective and affordable vaccines against these viruses. In 2023, researchers from the Shresta Lab received national honors for their dengue research and vaccine advances, winning the Alnylam Pharmaceuticals for Scientific Excellence Award; the Genentech Award for Justice, Diversity, Equity, and Inclusion; and the MilliporeSigma Award for Global Impact in the Nucleate Activator competition.
Learn more:
Related News
- Immune Matters
- Research News
- Research News
Research Projects
The Sette lab’s previous large scale epitope identification efforts (supported by HHS contracts) have led to a deeper understanding of the role of T cells and HLA variants in the [...]
The aim of this work, in collaboration with Bjoern Peters, Ph.D., and Pandurangan Vijayanand, M.D., Ph.D., is to characterize the immune response to dengue virus (DENV) and Mycobacterium tuberculosis (MTB), [...]