LA JOLLA, CA—Regulatory T cells (Treg cells) are part of the system of checks and balances that prevents the immune response from going overboard and causing autoimmune disease. Although critically important for shaping the immune response and maintaining self-‐tolerance, how they hold on to their immune-‐suppressive powers had remained unclear. Now, for the first time, researchers at the La Jolla Institute for Immunology identified a molecular pathway that maintains the stability and function of Treg cells.
Their findings, published in the June 16, 2015 issue of Immunity, pinpoint a protein degradation pathway, which acts as an oxygen sensor in many cell types, as a critical regulator of Treg cells’ function. When inactivated in Treg cells, they not only lost their immune-‐suppressive function, but started to produce inflammatory signals themselves, leading to massive inflammation throughout the body.
“Due to the inhibitory function of Treg cells, people have been trying to use these cells for therapy in human autoimmune diseases or transplantation,” explains professor Yun-‐Cai Liu, Ph.D., who led the current study. “Our results suggest that these cells may not be stable, and, under certain conditions, may be even converted into inflammatory cells.” He hopes that further studies may identify novel approaches to immune-‐based cancer therapy or reveal new drug targets for inflammatory diseases.
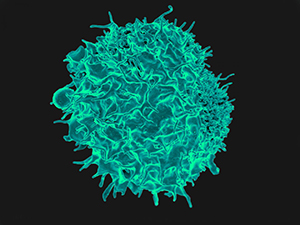
Liu and his team became interested in the phenomenon of Treg cell instability after earlier studies had hinted at Treg cells’ shape-‐shifting abilities but no specific molecular mechanism ensuring their functional stability—or lack thereof—had been identified. “Treg cells are concentrated in areas of low oxygen, conditions that are typically found at the center of a tumor mass or in inflamed tissue. Presumably, there they are exposed to hypoxia,” says postdoctoral researcher and first author Jeeho Lee, Ph.D.
Hypoxia-‐inducible factor 1〈 (HIF-‐1〈), an oxygen sensor that controls the expression of various genes for glucose metabolism under conditions of low oxygen levels, is the most well documented substrate of the von Hippel-‐Lindau (VHL) enzyme. Under normal oxygen conditions, VHL flags the protein for destruction by the cell’s protein disposal machinery. When oxygen is scarce, however, HIF-‐1〈 starts to accumulate and turns on the expression of a host of genes that assist in promoting and increasing oxygen delivery to hypoxic regions.
Earlier studies had implicated HIF-‐1〈 in the regulation of the immune system—with conflicting results. “We wanted to explore the role of HIF-‐1〈 by addressing the question in Treg cells directly,” says Lee.
When the LJI researchers genetically engineered Treg cells to lack VHL, the amount of HIF-‐1〈 within these cells, as expected, increased sharply. But, more importantly, the Treg cells became highly activated and started to produce large amounts of inflammatory cytokines, chemical messengers that are secreted by cells of the immune system to communicate with each other.
“The result was severe and widespread inflammation in many tissues and organs,” observes Lee. In addition, it shifted the cells’ glucose metabolism from aerobic to anaerobic. These changes resulted in the production of harmful metabolites that increase inflammation even further.
“Our studies imply that the change of oxygen levels in different tissues can be sensed by Treg cells and that this process is critically important for maintaining the correct balance between activation and suppression of the immune system,” says Liu.
The work was funded in part by the La Jolla Institute for Immunology, the National Institutes of Health (RO1AI62969, RO1AI178272 and PO1AI089624.)Full citation: “E3 ubiquitin ligase VHL regulates hypoxia-‐inducible factor-‐1〈 to maintain regulatory T cell stability and suppressive capacity.” Jee H. Lee, Chris Elly, Yoon Park and Yun-‐Cai Liu. Immunity 2015.
doi:10.1016/j.immuni.2015.05.016
ABOUT LA JOLLA INSTITUTE
La Jolla Institute for Immunology is dedicated to understanding the intricacies and power of the immune system so that we may apply that knowledge to promote human health and prevent a wide range of diseases. Since its founding in 1988 as an independent, nonprofit research organization, the Institute has made numerous advances leading towards its goal: life without disease→.


