COVID-19
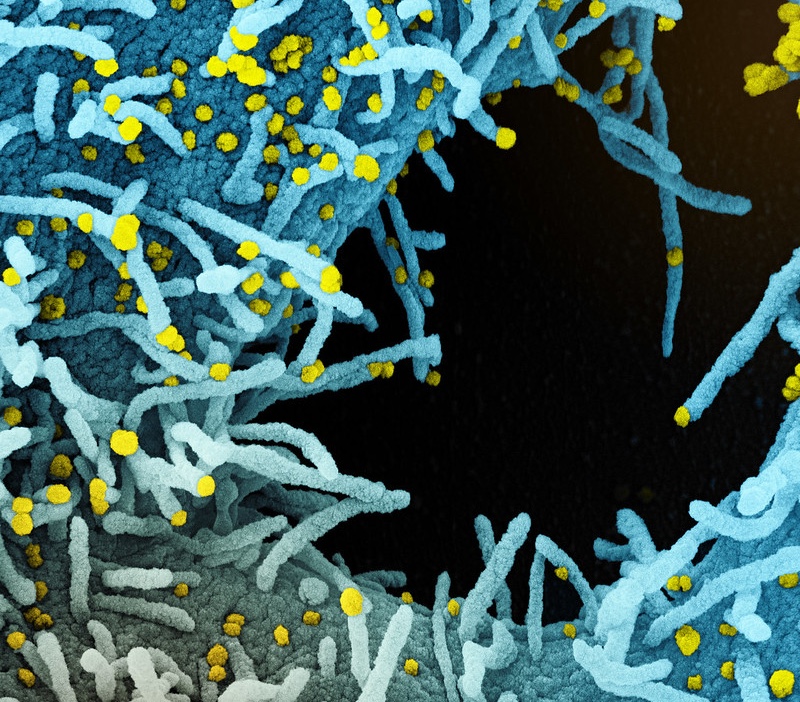
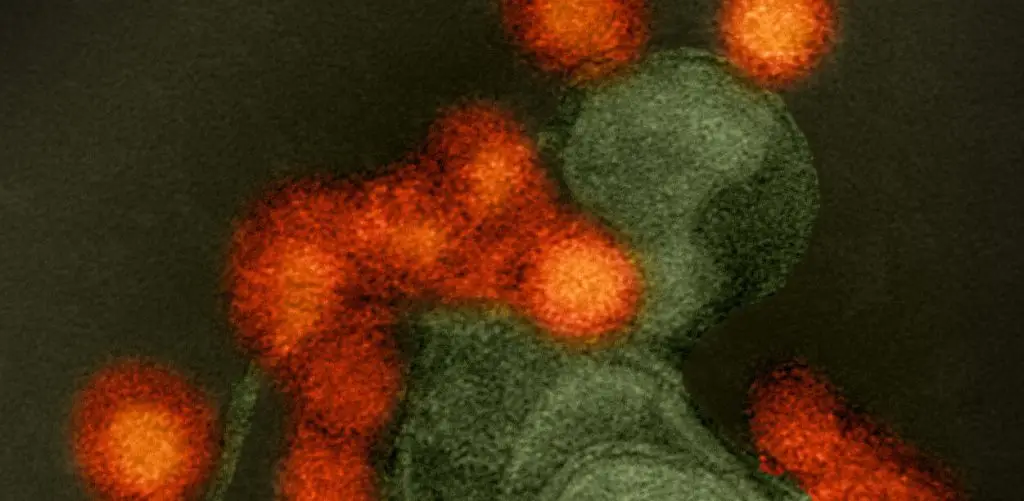
COVID-19 was first identified in late 2019. The virus that causes COVID-19 is called SARS-CoV-2. This virus spreads through airborne particles, droplets, and touching of the mucosal membranes with hands contaminated with the virus. It can be transmitted by asymptomatic or pre-symptomatic “carriers” of the disease.
SARS-CoV-2 is related to the same coronaviruses that cause the common cold. Patients who show signs of COVID-19 often experience flu-like symptoms that can escalate to severe breathing difficulty and death. The virus can also cause cardiovascular symptoms, such as stroke, and lasting lung damage. The virus can also cause a rare but serious complication called Multisystem Inflammatory Syndrome in Children (MIS-C) in younger patients.
[See full list of COVID-19 symptoms]
The COVID-19 pandemic led to research breakthroughs and massive global collaborations. The fast-paced effort to design vaccines against the virus led to multiple effective vaccines, and there are several experimental therapies that have saved countless lives. Researchers around the world have also come together to track the rise of new SARS-CoV-2 variants, which are mutated forms of the original virus. Some of these variants, such as the Omicron variants, have the potential to “escape” immunity and cause “breakthrough” infections in vaccinated people. This phenomenon has led scientists to develop new vaccine “boosters” to help the immune system better targeted the mutated virus.
In addition to protecting people from infection and death, researchers are working to understand the effects of “long COVID,” an unpredictable and debilitating range of symptoms that can last for months or years after the initial infection. People who have experienced severe cases of acute COVID-19 are at greater risk of developing long COVID, though anyone who has been infected is potentially vulnerable, according to the U.S. Centers for Disease Control and Prevention.
Our Approach
Scientists at La Jolla Institute for Immunology (LJI) remain at the forefront of research into COVID-19 vaccines, therapies, and the disease’s long-term effects.
Leading T cell breakthroughs
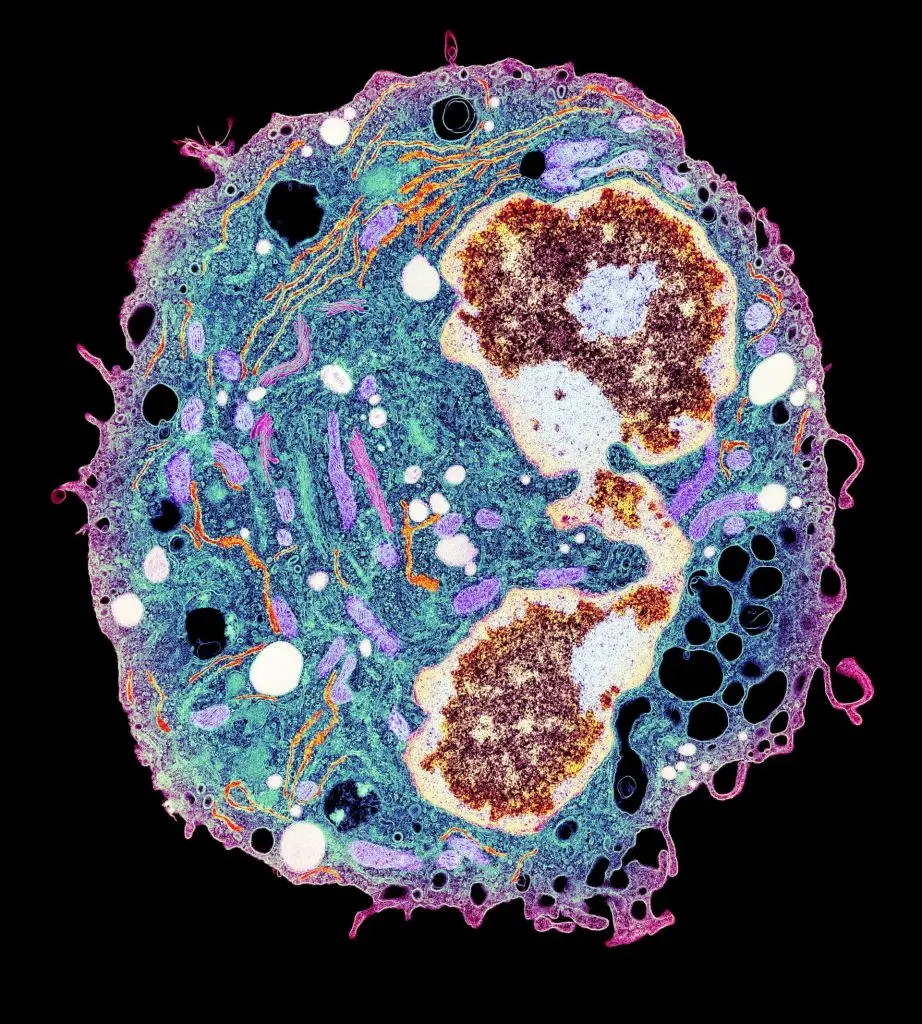
In January 2020, LJI scientists began studying T cell reactivity to the SARS-CoV-2 virus. Their findings gave the world early evidence that the immune system could indeed fight off the virus, offering hope that a vaccine could be effective.
LJI Professors Alessandro Sette, Dr.Biol.Sci., and Shane Crotty, Ph.D., continued this groundbreaking research throughout 2020 and 2021. Their labs were the first to share a detailed analysis of the body’s adaptive immune response to the virus. Importantly, they showed that people who had previously had common cold coronaviruses had “cross-reactive” T cells that also recognized SARS-CoV-2. Their labs also found that a dysfunctional T cell response could explain the huge variation in COVID-19 outcomes, especially in the elderly.
[More about this effort in the Immune Matters article “The world goes crazy around you”]
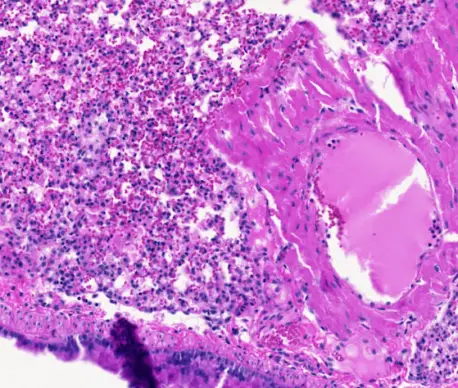
LJI Professor Pandurangan Vijayanand, M.D., Ph.D., worked with scientists at the University of Liverpool and the University of Southampton to show that people with severe COVID-19 cases may be left with more of the protective “memory” T cells needed to fight reinfection. The Vijayanand Lab also found that early in the illness, patients hospitalized with severe cases of COVID-19 develop a novel T cell subset that can potentially kill B cells and reduce antibody production.
As the Omicron SARS-CoV-2 variant spread in late 2021 and 2022, the Sette and Crotty Labs reported that COVID-19 vaccines could induce a strong T cell response against this variant. This work provided a clue to why vaccinated people were experiencing “breakthrough” infections but lower rates of severe illness. In May 2024, the Sette, Grifoni and Crotty Labs published new data showing how COVID-19 ‘breakthrough’ infections prompt people to develop T cells that are better at recognizing and targeting SARS-CoV-2, including the Omicron and Delta variants. Their findings, published in Cell Reports Medicine, suggest repeated vaccination and infection leads T cells and B cells to build an “immunity wall.”
In 2023, Drs. Sette and Grifoni published further research on cross-reactive T cells. Their work showed that T cells can indeed recognize several different viral targets, called “antigens,” shared between most coronaviruses, including common cold coronaviruses and SARS-CoV-2. They also looked more in-depth at what fragments of these antigens, called “epitopes,” are recognized and how conserved they are across different coronaviruses. These findings may help the development of pan-coronavirus vaccines.
Drs. Sette and Grifoni went on to publish a 2024 study where they used bioinformatics tools to predict T cell reactivity to the newly circulating SARS-CoV-2 “Pirola” variant. Their analysis suggested T cell immunity to previous SARS-CoV-2 expose or SARS-CoV-2 immunization should help combat the Pirola variant as well.
In a 2024 study, LJI Professor Sujan Shresta, Ph.D., published direct evidence that exposure to common cold coronaviruses can train T cells to fight SARS-CoV-2. In fact, prior exposure to a common cold coronavirus appears to partially protect mice from lung damage during a subsequent SARS-CoV-2 infection. The Shresta Laboratory is now working to develop novel vaccines purposefully designed to harness these cross-reactive T cells and protect against SARS-CoV-2 and several other coronaviruses with pandemic potential.
Fueling vaccine development
By early 2021, LJI scientists had shown that COVID-19 survivors held on to SARS-CoV-2 immunity for at least eight months. The Crotty and Sette Labs then found that Pfizer-BioNTech and Moderna vaccines effectively prime T cells to fight SARS-CoV-2 variants. A key study, co-led by LJI Research Assistant Professor Alba Grifoni, Ph.D., showed exactly how these T cells can mount attacks against many SARS-CoV-2 targets—even on new virus variants. This work was key for understanding how people around the world may respond to emerging SARS-CoV-2 variants.
LJI Assistant Professor Daniela Weiskopf, Ph.D., co-led research suggesting even a low dose of the Moderna vaccine lasts for at least six months. This study in Science also showed that cross-reactive T cells from previous common cold coronavirus infections can help a vaccinated person fight the virus.
By 2022, LJI researchers were on the forefront of studying how the immune system responds to the different types of COVID-19 vaccines available. In May 2022, LJI scientists published first head-to-head comparison of four COVID-19 vaccines, which revealed the strength of T cell, B cell, and antibody responses over time.
LJI scientists have also pioneered new research methods to advance the development of intranasal vaccines against COVID-19 and other respiratory diseases. In 2024, Dr. Crotty and LJI Postdoctoral Research Sydney Ramirez, Ph.D., published the first-ever, in-depth analysis of immune cell activity in the upper airway. Their investigation revealed a strong population of “tissue resident” memory cells, which stand ready to defend the airway from SARS-CoV-2.The scientists say these findings may lead to better vaccines to boost immune protection in the airways.
Guiding COVID-19 therapeutics
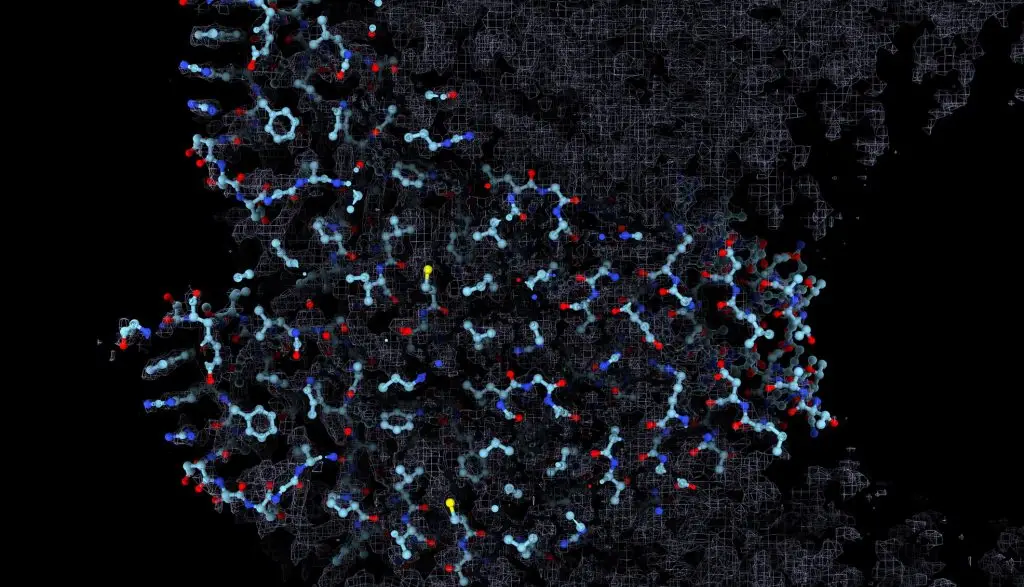
In 2020, LJI Professor, President, and CEO Erica Ollmann Saphire, Ph.D., MBA, launched the Coronavirus Immunotherapeutic Consortium (CoVIC), with backing from the Bill & Melinda Gates Foundation. With more than 50 different efforts currently underway to find therapeutic antibodies across the globe, CoVIC provides a coordinated and standardized effort to compare these antibody candidates side by side. In September 2021, CoVIC published a study in Science highlighting key details of where SARS-CoV-2 is vulnerable and which antibody “all stars” could be combined in life-saving therapies.
In 2023, the Saphire Lab published an important discovery: Instead of targeting a single binding site on the SARS-CoV-2 Spike protein, powerful neutralizing antibodies bind to two vulnerable sites at once. Through this “bivalent” binding, the antibodies can lock key viral structures into position, preventing the virus from infecting host cells. In the study, these bivalent antibodies appeared to retain efficacy against both early SARS-CoV-2 variants and several later Omicron variants.
The Saphire Lab also showed how the original Moderna SARS-CoV-2 vaccine could prompt the body to produce antibodies against the later Omicron variants of SARS-CoV-2. The researchers also captured highly detailed, 3D structures of three promising neutralizing antibodies bound to Spike. This important work shows exactly where Spike is vulnerable to human antibodies—and how future vaccines and antibody therapeutics might exploit these weaknesses.
The Vijayanand Lab also shed light on how key genetic differences leave some patients at a disadvantage when fighting COVID-19. The team found that a gene in a cell type called non-classical monocytes, which are part of the body’s “first responder” team of innate immune cells, could be a potential target for COVID-19 therapies.
Embracing collaboration
Work between the Saphire Lab and researchers at Los Alamos National Laboratory also gave us an early look at how SARS-CoV-2 was mutating as it spread across the globe, alerting many to the development of viral variants.
A collaboration between the Saphire, Sette, Crotty Labs, alongside scientists at Columbia University, also led to the discovery that the lungs of COVID-19 survivors teem with virus-fighting ‘memory’ cells. The scientists spotted specialized sites, called germinal centers—where antibody-producing B cells and memory B cells are generated—within the lung-associated lymph nodes for up to six months after infection, even in elderly individuals. Thanks to these germinal centers, B cells continue to produce antibodies against SARS-CoV-2 and the body can continue to hone its immune response to the virus.
Going forward
LJI scientists are building on these accomplishments.
Dr. Shresta has won funding to study the spread of COVID-19 in Nepal, Vietnam, and the Philippines. These new projects will shed light on how infectious diseases spread in these countries—and how differences in geography and genetics affect immune responses. She is also working with Charles Rivers Laboratories to develop additional mouse models to study how the human immune system fights SARS-CoV-2. In 2024, the Shresta Lab published a collaboration with Synbal Inc., showing how a new, “humanized” mouse models can shed light on how SARS-CoV-2 moves through the body—and why different people experience wildly different COVID-19 symptoms.
LJI Professor Sonia Sharma, Ph.D., has established new collaborations to study children afflicted with MIS-C. She and her team are using samples collected from children and adults in the Los Angeles area to examine whether the same immune-related metabolic mechanisms underlie multi-organ inflammation and vasculitis in children with MIS-C.
Dr. Peters and his team have been working on data standardization and analysis for the largest NIH study of COVID-induced immune responses to date. His lab has been following patients for over 12 months to track the effects of COVID infections, including long COVID.
Dr. Weiskopf has been granted $1.4 million from the National Institutes of Health’s National Cancer Institute (NCI) to examine the immune response to SARS-CoV-2 in study volunteers from Puerto Rico, where at least 75 percent of the population identifies as Hispanic or Latino.
LJI Postdoctoral Associate Sydney Ramirez, Ph.D., won a three-year fellowship from the A.P. Giannini Foundation to study adaptive immunity to SARS-CoV-2. She wants to know how the development of SARS-CoV-2-specific B cell and T cell immunity in acute cases of COVID-19 correlates with viral loads, symptoms and disease severity.
Vaccine research at the Institute continues with studies of how people respond to different COVID-19 vaccine platforms and how these vaccines protect against severe illness from SARS-CoV-2 variants. Dr. Saphire and her team have also received more than $2.6 million in funding from the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, to help develop a pan-coronavirus vaccine that could be effective for years to come.
Related News
- Immune Matters
- Immune Matters
- Research News
Research Projects
Selected References Kusnadi A, Ramírez-Suástegui C, Fajardo V, Chee SJ, Meckiff BJ, Simon H, Pelosi E, Seumois G, Ay F, Vijayanand P, Ottensmeier CH. Severely ill COVID-19 patients display [...]
As the SARS-CoV-2 related disease COVID-19 hit hard and changed the lives of every person on earth, the Vijayanand lab recently started to put their expertise in single-cell analysis [...]
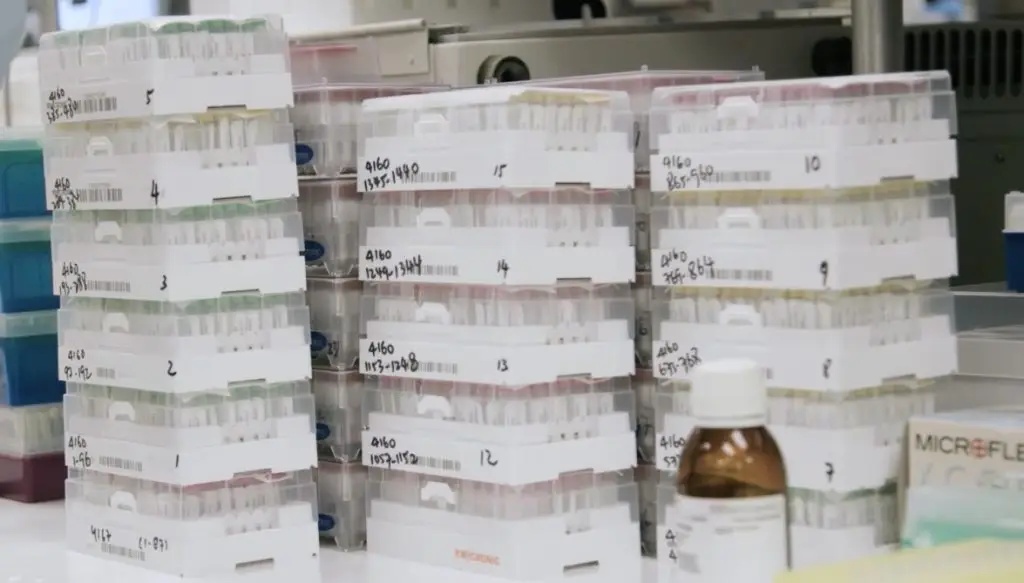
COVIC-DB: To co-run the LJI-led CoVIC database in the effort to find ideal therapeutic combinations for the novel coronavirus, the assays that best predict efficacy, and the features that provide [...]