Our Approach
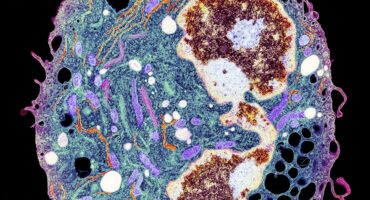
Scientists at La Jolla Institute for Immunology (LJI) are studying the genetic causes and cellular response to allergens in an effort to make allergic immunotherapeutics more efficient and even tailored to specific patients.
LJI Professor Toshiaki Kawakami, M.D., Ph.D., has been studying allergic diseases at the basic as well as clinically relevant levels. His group has revealed the secret of a secreted protein named histamine-releasing factor (HRF) as an essential pro-inflammatory effector in asthma and food allergy. They have generated inhibitors of HRF that can prevent these diseases in animals and are now working to translate these inhibitors to human diseases. Dr. Kawakami is also interested in signaling transduction of mast cell activation and developing better animal models of allergic diseases. In the past his laboratory devised a way to induce a condition similar to the allergic disease atopic dermatitis in mice.
LJI Professors Alessandro Sette, Dr. Biol. Sci., and Bjoern Peters, Ph.D., are working to identify the sites on allergen molecules that trigger an inflammatory immune response. They have been working on a variety of different allergens, including milk and peanut allergens, pollens, fungi, dust mites, mice and cockroach allergens. Apart from the experimental work they also lead a free, online resource called the Immune Epitope Database (IEDB), which collects and shares allergen data with scientists around the world.
Dr. Sette is also investigating cockroach allergy, which is a major contributor to asthma development in urban settings. As part of a large NIH-funded effort to develop immunotherapies for this allergy (the Inner City Asthma Consortium, or ICAC), the Sette lab efforts characterize T cell responses in allergic individuals before and after immunotherapy.
And researchers in Dr. Peters’s lab have analyzed immune cells in dozens of blood samples from allergy patients receiving allergy shots. Their work has shown that allergy immunotherapy shifts the balance between two types of immune cells: those that help churn out antibodies and those that knock down antibody production. As the latter gain the upper hand, the flood of allergy-associated IgE antibodies gradually decreases and patients’ symptoms start to improve. Currently, Dr. Peters is researching how these and other findings in inhaled allergens translate to food allergies, specifically those that affect children.
LJI Professor Pandurangan Vijayanand, M.D., Ph.D., focuses on using genomic and epigenomic tools to understand the molecular basis of asthma. His laboratory has developed techniques to study the molecular profiles of circulating and airway immune cells from patients with asthma and other diseases, using fewer cells than was possible previously. He aims to understand the epigenetic and genetic variations that contribute to a person’s susceptibility to diseases like asthma, lung cancer, and other pulmonary diseases.
Working with LJI Research Assistant Professor Grégory Seumois, Ph.D., Dr. Vijayanand recently found that a previously unknown population of T cells may help “dampen” the allergic response to house dust mites, a very common cause of allergies and asthma. This finding suggests that there may be a way to boost this T cell population to reduce responses to house dust mites and other allergens.